Overdose and Overdose Mortality
The US Centers for Disease Control reports, using provisional data available for analysis on June 1, 2025, that in calendar year 2024 at least 80,112 people in the US are reported to have died from drug overdose and toxins in the unregulated drug supply. These provisional data are incomplete and the CDC predicts that the final number of deaths in the US due to overdose and toxins in the unregulated drug supply in calendar year 2024 will be 80,719.
- In the 12-month period ending January 31, 2025, at least 77,677 people in the US were reported to have died from drug overdose and toxins in the unregulated drug supply. The CDC predicts that the final number of overdose deaths in that period will be 82,138.
- In calendar year 2023, at least 106,881 people in the US were reported to have died from drug overdose and toxins in the unregulated drug supply. The CDC predicts that the final number of overdose deaths in calendar year 2023 will be 110,037.
- In calendar year 2022, at least 109,413 people in the US were reported to have died from drug overdose and toxins in the unregulated drug supply. The CDC predicts that the final number of overdose deaths in calendar year 2022 will be 112,582.
- In calendar year 2021, at least 107,573 people in the US were reported to have died from drug overdose and toxins in the unregulated drug supply. The CDC predicts that the final number of overdose deaths in calendar year 2021 will be 110,697.
Source: Ahmad FB, Cisewski JA, Rossen LM, Sutton P. Provisional drug overdose death counts. Centers for Disease Control, National Center for Health Statistics. 2025. Last accessed June 11, 2025.
1. Deaths in the US Due to the Toxic Unregulated Drug Supply and Overdose, 1999-2023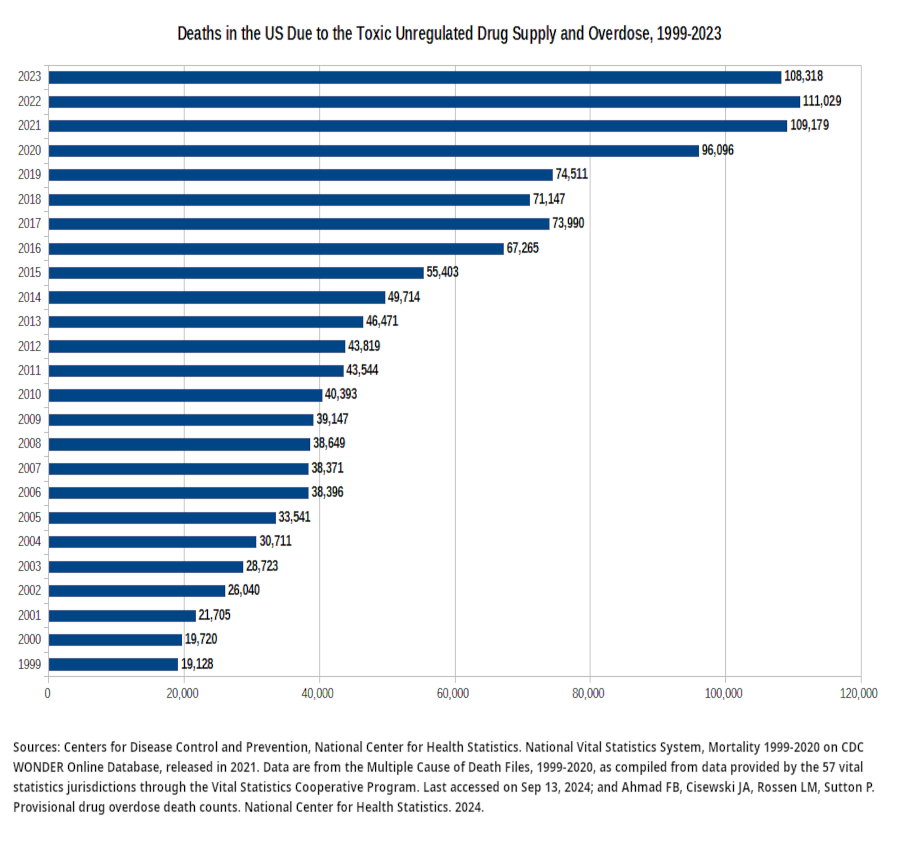 |
| 2. Deaths in the US in 2022 Due to a Toxic Unregulated Drug Supply and Overdose "● In 2022, 107,941 drug overdose deaths occurred, resulting in an age-adjusted rate of 32.6 deaths per 100,000 standard population (Figure 1). "● Overall, the age-adjusted rate of drug overdose deaths nearly quadrupled from 8.2 in 2002 to 32.6 in 2022; however, the rate did not significantly change between 2021 (32.4) and 2022 (32.6). "● Between 2021 and 2022, the age-adjusted rate of drug overdose deaths for males increased 1.1% from 45.1 to 45.6, while the rate for females decreased 1.0% from 19.6 to 19.4, although this decrease was not significant. Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. NCHS Data Brief, no 491. Hyattsville, MD: National Center for Health Statistics. 2024. DOI: dx.doi.org/10.15620/cdc:135849 |
| 3. Overdose Education and Naloxone Distribution (OEND) Within Syringe Service Programs (SSPs) "Among the 342 known SSPs operating at the beginning of 2019, 263 (77%) responded to the online survey; of these, 247 (94%) had an OEND program, 160 (65%) of which had been implemented since 2016 (Figure 1). With regard to phases of OEND implementation, 173 (66%) responding SSPs had been implementing OEND for 12 months or more, 74 (28%) had implemented OEND within the last 12 months, eight (3%) were actively preparing for OEND implementation, and eight (3%) were exploring OEND implementation (Table). Of the 16 SSPs not yet offering OEND, four had previously implemented naloxone distribution but stopped because of an inadequate naloxone supply or funding. "Among the 247 SSPs with an OEND program, 191 (77%) offered OEND every time syringe services were offered, and 214 (87%) provided naloxone refills as often as participants requested them (Table). SSPs reported offering OEND for a median of 15 of the past 28 days. Only 29 (12%) SSPs entered OEND data directly into an electronic data system. During the preceding 12 months, 237 (96%) of 247 SSPs with OEND programs reported distributing 702,232 naloxone doses, including refills, to 230,506 persons (an average of 3 doses per person). Sixty-two (26%) SSPs reported distributing naloxone to >1,000 persons in the last 12 months; these programs had distributed naloxone to 186,603 laypersons, who represented 81% of all recipients in the past 12 months. Overall, 14 (6%) SSPs reported distribution of ≥10,000 naloxone doses during the last 12 months, accounting for 382,132 naloxone doses, 54% of all doses distributed by SSPs in the past 12 months. These 14 SSPs are located throughout six of the nine census divisions. Seventy-two (29%) SSPs ran out of naloxone or needed to ration their naloxone in the preceding 3 months." Lambdin, B. H., Bluthenthal, R. N., Wenger, L. D., Wheeler, E., Garner, B., Lakosky, P., & Kral, A. H. (2020). Overdose Education and Naloxone Distribution Within Syringe Service Programs - United States, 2019. MMWR. Morbidity and mortality weekly report, 69(33), 1117–1121. doi.org/10.15585/mmwr.mm6933a2 |
| 4. Emergency Department Visits and Trends Related to Cocaine, Psychostimulants, and Opioids in the United States, 2008–2018 "Psychostimulant-related ED visits increased from 2.2 to 12.9 visits per 10,000 population from 2008 to 2018. This is consistent with studies showing increasing national rates of ED visits, hospitalizations, and deaths from psychostimulant overdose [2, 4, 5, 33]. The increasing use of the ED and other acute care settings is likely linked to rising methamphetamine availability and use [34]. National Forensic Laboratory Information System data found methamphetamine case submissions increased from 2011 to 2019, with methamphetamine as the most frequently reported drug [35]. While psychostimulant-related ED visits were predominantly among Western regions in our study, recent data highlights the emergence of psychostimulant-related overdose deaths in the Midwest and Northeast, suggesting methamphetamine is already a nationwide concern [8, 36]. Increases in cocaine-related ED visits were not significant, potentially due to the exclusion of visits related to opioid and cocaine co-use. Polysubstance use is common in among individuals using cocaine [30], and other studies found rates of fatal overdoses and ED visits for overdose involving cocaine and opioid use are rising [5, 33]. "We found stimulant-related ED visits were less likely to be identified as drug toxicity/withdrawal concerns, underscoring the differences in presentations between stimulant- and opioid-related visits. While the national surge in ED visits and deaths related to opioid overdose is linked to the rise in fentanyl in the drug supply [1, 33, 37], the main drivers of stimulant-related ED visits and overdoses are unclear. Possibilities include increased potency of fluctuating drug supplies [35], contamination or co-use with synthetic opioids like fentanyl [38], or the cumulative effects of chronic stimulant use over time [39]. Further, the term “overdose”, when applied to opioids commonly refers to an acute respiratory event from an episode of use, and this term is problematic when applied to stimulants, as it lacks specificity in capturing the diverse ways in which stimulant toxicity can present [16, 40]. Our data suggest that acute emergency presentations related to stimulant use are more likely due to the cumulative effect of stimulant use over time rather than from a single episode of use. Addressing acute stimulant toxicity may rely more on clinical management of various symptoms, rather than the development of a single reversal agent like naloxone for opioid overdose." Suen, L.W., Davy-Mendez, T., LeSaint, K.T. et al. Emergency department visits and trends related to cocaine, psychostimulants, and opioids in the United States, 2008–2018. BMC Emerg Med 22, 19 (2022). doi.org/10.1186/s12873-022-00573-0. |
| 5. Drug Overdose Rates In The US, 2019 "The age-adjusted rate for drug overdose deaths in the United States for 2019 was 21.6 per 100,000 standard population (Figure 1, Table). The five states with the highest rates were West Virginia (52.8), Delaware (48.0), District of Columbia (43.2), Ohio (38.3), and Maryland (38.2). The five states with the lowest rates were Nebraska (8.7), South Dakota (10.5), Texas (10.8), North Dakota (11.4), and Iowa (11.5). "The age-adjusted drug overdose death rate for the non-Hispanic white population in 2019 (26.2 per 100,000 standard population) was 21.3% higher than the national rate (Figure 2). The rate for the non-Hispanic black population (24.8) was 14.8% higher than the national rate. The rate for the non-Hispanic American Indian or Alaska Native population (30.5) was 41.2% higher than the national rate. The rate for the non-Hispanic Asian population (3.3) was 84.7% lower than the national rate. The rate for the non-Hispanic Native Hawaiian or Other Pacific Islander population (9.5) was 56.0% lower than the national rate. The rate for the Hispanic population (12.7) was 41.2% lower than the national rate." Miniño AM, Hedegaard H. Drug poisoning mortality, by state and by race and ethnicity: United States, 2019. NCHS Health E-Stats. 2021. |
| 6. Deaths Attributed To Drug Overdose In The US In 2018 "● In 2018, there were 67,367 drug overdose deaths in the United States, a 4.1% decline from 2017 (70,237 deaths). "● The age-adjusted rate of drug overdose deaths in 2018 (20.7 per 100,000) was 4.6% lower than in 2017 (21.7). "● For 14 states and the District of Columbia, the drug overdose death rate was lower in 2018 than in 2017. "● The rate of drug overdose deaths involving synthetic opioids other than methadone (drugs such as fentanyl, fentanyl analogs, and tramadol) increased by 10%, from 9.0 in 2017 to 9.9 in 2018. "● From 2012 through 2018, the rate of drug overdose deaths involving cocaine more than tripled (from 1.4 to 4.5) and the rate for deaths involving psychostimulants with abuse potential (drugs such as methamphetamine) increased nearly 5-fold (from 0.8 to 3.9)." Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, no 356. Hyattsville, MD: National Center for Health Statistics. 2020. |
| 7. Unprecedented Increases In Overdose Mortality In First Seven Months Of 2020 "By disaggregating monthly trends, we found that unprecedented increases in overdose mortality occurred during the early months of pandemic in the United States. At the peak, overdose deaths in May 2020 were elevated by nearly 60% compared with the previous year, and the first 7 months of 2020 were overall elevated by 35% compared with the same period for 2019. To put this in perspective, if the final values through December 2020 were to be elevated by a similar margin, we would expect a total of 93,000 to 98,000 deaths to eventually be recorded for the year. Values for the remaining 5 months of 2020 have yet to be seen; however, it is very likely that 2020 will represent the largest year-to-year increase in overdose mortality in recent history for the United States." Joseph Friedman , Samir Akre , “COVID-19 and the Drug Overdose Crisis: Uncovering the Deadliest Months in the United States, January‒July 2020”, American Journal of Public Health 111, no. 7 (July 1, 2021): pp. 1284-1291. |
| 8. Deaths in 2017 in the US Attributed to Drug Overdose " In 2017, there were 70,237 drug overdose deaths in the United States. " The age-adjusted rate of drug overdose deaths in 2017 (21.7 per 100,000) was 9.6% higher than the rate in 2016 (19.8). " Adults aged 25–34, 35–44, and 45–54 had higher rates of drug overdose deaths in 2017 than those aged 15–24, 55–64, and 65 and over. " West Virginia (57.8 per 100,000), Ohio (46.3), Pennsylvania (44.3), and the District of Columbia (44.0) had the highest age-adjusted drug overdose death rates in 2017. " The age-adjusted rate of drug overdose deaths involving synthetic opioids other than methadone (drugs such as fentanyl, fentanyl analogs, and tramadol) increased by 45% between 2016 and 2017, from 6.2 to 9.0 per 100,000." Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief, no 329. Hyattsville, MD: National Center for Health Statistics. 2018. |
| 9. Changes in Synthetic Opioid Involvement in Overdose Deaths in the US and Involvement of Other Drugs in Combination "Among the 42,249 opioid-related overdose deaths in 2016, 19,413 involved synthetic opioids, 17,087 involved prescription opioids, and 15,469 involved heroin. Synthetic opioid involvement in these deaths increased significantly from 3007 (14.3% of opioid-related deaths) in 2010 to 19,413 (45.9%) in 2016 (P for trend <.01). Significant increases in synthetic opioid involvement in overdose deaths involving prescription opioids, heroin, and all other illicit or psychotherapeutic drugs were found from 2010 through 2016 (Table). "Among synthetic opioid–related overdose deaths in 2016, 79.7% involved another drug or alcohol. The most common co-involved substances were another opioid (47.9%), heroin (29.8%), cocaine (21.6%), prescription opioids (20.9%), benzodiazepines (17.0%), alcohol (11.1%), psychostimulants (5.4%), and antidepressants (5.2%) (Figure)." Jones CM, Einstein EB, Compton WM. Changes in Synthetic Opioid Involvement in Drug Overdose Deaths in the United States, 2010-2016. JAMA. 2018;319(17):1819–1821. |
| 10. Deaths in the US in 2022 Involving Cocaine or Stimulants "● The age-adjusted rate of drug overdose deaths involving cocaine increased slightly from 1.6 deaths per 100,000 standard population in 2002 to 2.5 in 2006, decreased to 1.3 in 2010, then increased to 8.2 in 2022; the rate in 2022 was 12.3% higher than the rate in 2021 (7.3) (Figure 5). "● The age-adjusted rate of drug overdose deaths involving psychostimulants with abuse potential (subsequently, psychostimulants), which includes methamphetamine, amphetamine, and methylphenidate, was 4.0% higher in 2022 than the rate in 2021 (10.4 compared with 10.0). "● The age-adjusted rate of drug overdose deaths involving psychostimulants increased more than 34 times from 2002 (0.3) to 2022 (10.4), with different rates of change over time." Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. NCHS Data Brief, no 491. Hyattsville, MD: National Center for Health Statistics. 2024. DOI: dx.doi.org/10.15620/cdc:135849 |
| 11. Decriminalization and Deaths from a Toxic Unregulated Drug Supply and Overdose "Oregon and Washington have recently made changes to their drug laws to fully or partially legalize possession of small amounts of drugs and increase investment in treatment access. To our knowledge, this is the first study to evaluate the association between those changes and fatal drug overdose. Using the synthetic control method to compare post-drug policy changes in fatal drug overdose rates in Oregon and Washington and estimated rates in the absence of these drug policy changes, we found no evidence that either Measure 110 in Oregon or the Washington Blake decision and subsequent legislative amendments were associated with changes in fatal drug overdose rates in either state. These findings were also robust to variations in the donor pool and the modeling strategy." Joshi S, Rivera BD, Cerdá M, et al. One-Year Association of Drug Possession Law Change With Fatal Drug Overdose in Oregon and Washington. JAMA Psychiatry. Published online September 27, 2023. doi:10.1001/jamapsychiatry.2023.3416 |
| 12. Drug Poisoning Deaths In The US, 2019 "In 2019, 70,630 deaths from the toxic effects of drug poisoning (drug overdose) occurred in the United States (1), a 4.8% increase compared with 2018 and the highest recorded number in recent history." Miniño AM, Hedegaard H. Drug poisoning mortality, by state and by race and ethnicity: United States, 2019. NCHS Health E-Stats. Centers for Disease Control, National Center for Health Statistics, 2021. |
| 13. Naloxone "Naloxone has been used as an antidote to opioids for over 50 years, and the drug has been readily available as a parenteral formula. Naloxone acts as a pure μ-opioid receptor competitive antagonist and is instrumental in preventing accidental overdose of opioids. Due to its effectiveness in preventing death due to opioid overdose, the federal government has recommended that naloxone should be available over-the-counter at most pharmacies. Naloxone can be obtained without a prescription in 43 states and can be administered by emergency medical personnel and law enforcement officials. With the availability of naloxone over the counter, it is now easier for family members and caregivers of patients with opioid use disorder to administer naloxone and potentially save lives.[1]" Jordan MR, Patel P, Morrisonponce D. Naloxone. [Updated 2024 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. |
| 14. Co-Involvement of Stimulants and Fentanyl in Drug-Related Deaths in the US, 2010-2021 "Findings "The percent of US overdose deaths involving both fentanyl and stimulants increased from 0.6% (n = 235) in 2010 to 32.3% (34 429) in 2021, with the sharpest rise starting in 2015. In 2010, fentanyl was most commonly found alongside prescription opioids, benzodiazepines, and alcohol. In the Northeast this shifted to heroin-fentanyl co-involvement in the mid-2010s, and nearly universally to cocaine-fentanyl co-involvement by 2021. Universally in the West, and in the majority of states in the South and Midwest, methamphetamine-fentanyl co-involvement predominated by 2021. The proportion of stimulant involvement in fentanyl-involved overdose deaths rose in virtually every state 2015–2021. Intersectional group analysis reveals particularly high rates for older Black and African American individuals living in the West. "Conclusions "By 2021 stimulants were the most common drug class found in fentanyl-involved overdoses in every state in the US. The rise of deaths involving cocaine and methamphetamine must be understood in the context of a drug market dominated by illicit fentanyls, which have made polysubstance use more sought-after and commonplace. The widespread concurrent use of fentanyl and stimulants, as well as other polysubstance formulations, presents novel health risks and public health challenges." Friedman, J, Shover, CL. Charting the fourth wave: Geographic, temporal, race/ethnicity and demographic trends in polysubstance fentanyl overdose deaths in the United States, 2010–2021. Addiction. 2023. doi.org/10.1111/add.16318 |
| 15. Routes of Administration and Deaths from Toxic Drug Supply and Drug Overdose "From January–June 2020 to July–December 2022, the number of overdose deaths with evidence of smoking doubled, and the percentage of deaths with evidence of smoking increased across all geographic regions. By late 2022, smoking was the predominant route of use among drug overdose deaths overall and in the Midwest and West regions. Increases were most pronounced when IMFs were detected, with or without stimulants. Increases in the number and percentage of deaths with evidence of smoking, and the corresponding decrease in those with evidence of injection, might be partially driven by 1) the transition from injecting heroin to smoking IMFs [Illicitly Manufactured Fentanyl] (3,4), 2) increases in deaths co-involving IMFs and stimulants that might be smoked†††† (1), and 3) increases in the use of counterfeit pills, which frequently contain IMFs and are often smoked (7). Motivations for transitioning from injection to smoking include fewer adverse health effects (e.g., fewer abscesses), reduced cost and stigma, sense of more control over drug quantity consumed per use (e.g., smoking small amounts during a period versus a single injection bolus), and a perception of reduced overdose risk among persons who use drugs (3,5,8). These motivations might also signify lower barriers for initiating drug use by smoking, or for transitioning from ingestion to smoking; compared with ingestion, smoking can intensify drug effects and increase overdose risk (9). Despite some risk reduction associated with smoking compared with injection (e.g., fewer bloodborne infections), smoking carries substantial overdose risk because of rapid drug absorption (5,9). "Nearly 80% of overdose deaths with evidence of smoking had no evidence of injection; persons who use drugs by smoking but do not inject drugs might not use traditional syringe services programs where harm reduction messaging and supplies are often provided. In response, some jurisdictions have adapted harm reduction services to provide safer smoking supplies or established health hubs to expand reach to persons using drugs through noninjection routes.§§§§ In addition, harm reduction services (e.g., peer outreach and provision of fentanyl test strips for testing drug products and naloxone to reverse opioid overdoses), messaging specific to smoking drugs, and linkage to treatment for substance use disorders can be integrated into other health care delivery (e.g., emergency departments) and public safety (e.g., drug diversion) settings. "The percentage and number of deaths with evidence of injection decreased across regions and drug categories. Observed decreases might reflect transitions to noninjection routes and response to public health efforts to reduce injection drug use because of its risk for overdose and infectious disease transmission (3,4,10). Despite these declines, more than 4,000 drug overdose deaths had evidence of injection during July–December 2022. Syringe services programs help to engage persons who use drugs in services (10); sustained efforts to provide sterile injection supplies, additional harm reduction tools, and linkage to treatment for substance use disorders, including medications for opioid use disorder, are important for further reduction in the number of overdose deaths from injection drug use. Lessons learned from implementing syringe services programs could be applied to other harm reduction and outreach models to reach more persons who use drugs by any route." Tanz LJ, Gladden RM, Dinwiddie AT, et al. Routes of Drug Use Among Drug Overdose Deaths — United States, 2020–2022. MMWR Morb Mortal Wkly Rep 2024;73:124–130. DOI: dx.doi.org/10.15585/mmwr.mm7306a2 |
| 16. Key Factors Underlying Increasing Rates of Heroin Use and Opioid Overdose in the US "A key factor underlying the recent increases in rates of heroin use and overdose may be the low cost and high purity of heroin.45,46 The price in retail purchases has been lower than $600 per pure gram every year since 2001, with costs of $465 in 2012 and $552 in 2002, as compared with $1237 in 1992 and $2690 in 1982.45 A recent study showed that each $100 decrease in the price per pure gram of heroin resulted in a 2.9% increase in the number of hospitalizations for heroin overdose.46" Wilson M. Compton, M.D., M.P.E., Christopher M. Jones, Pharm.D., M.P.H., and Grant T. Baldwin, Ph.D., M.P.H. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N Engl J Med 2016; 374:154-163. January 14, 2016. DOI: 10.1056/NEJMra1508490. |
| 17. Drug Overdose Deaths In 2018 - Demographic Details and Changes from 2017 "During 2018, drug overdoses resulted in 67,367 deaths in the United States, a 4.1% decrease from 2017. Among these drug overdose deaths, 46,802 (69.5%) involved an opioid. From 2017 to 2018, opioid-involved death rates decreased 2.0%, from 14.9 per 100,000 population to 14.6 (Table 1); decreases occurred among females; persons aged 15–34 years and 45–54 years; non-Hispanic whites; and in small metro, micropolitan, and noncore areas; and in the Midwest and South regions. Rates during 2017–2018 increased among persons aged ≥65 years, non-Hispanic blacks, and Hispanics, and in the Northeast and the West regions. Rates decreased in 11 states and DC and increased in three states, with the largest relative (percentage) decrease in Iowa (–30.4%) and the largest absolute decrease (difference in rates) in Ohio (–9.6); the largest relative and absolute increase occurred in Missouri (18.8%, 3.1). The highest opioid-involved death rate in 2018 was in West Virginia (42.4 per 100,000). "Prescription opioid-involved death rates decreased by 13.5% from 2017 to 2018. Rates decreased in males and females, persons aged 15–64 years, non-Hispanic whites, Hispanics, non-Hispanic American Indian/Alaska Natives, and across all urbanization levels. Prescription opioid–involved death rates remained stable in the Northeast and decreased in the Midwest, South, and the West. Seventeen states experienced declines in prescription opioid–involved death rates, with no states experiencing significant increases. The largest relative decrease occurred in Ohio (–40.5%), whereas the largest absolute decrease occurred in West Virginia (–4.1), which also had the highest prescription opioid-involved death rate in 2018 (13.1 per 100,000). "Heroin-involved death rates decreased 4.1% from 2017 to 2018; reductions occurred among males and females, persons aged 15–34 years, non-Hispanic whites, and in large central metro and large fringe metro areas (Table 2). Rates decreased in the Midwest and increased in the West. Rates decreased in seven states and DC and increased in three states from 2017 to 2018. The largest relative decrease occurred in Kentucky (50.0%), and the largest absolute decrease occurred in DC (–7.1); the largest relative and absolute increase was in Tennessee (18.8%, 0.9). The highest heroin-involved death rate in 2018 was in Vermont (12.5 per 100,000). "Death rates involving synthetic opioids increased from 9.0 per 100,000 population in 2017 to 9.9 in 2018 and accounted for 67.0% of opioid-involved deaths in 2018. These rates increased from 2017 to 2018 among males and females, persons aged ≥25 years, non-Hispanic whites, non-Hispanic blacks, Hispanics, non-Hispanic Asian/Pacific Islanders, and in large central metro, large fringe metro, medium metro, and small metro counties. Synthetic opioid–involved death rates increased in the Northeast, South and West and remained stable in the Midwest. Rates increased in 10 states and decreased in two states. The largest relative increase occurred in Arizona (92.5%), and the largest absolute increase occurred in Maryland and Missouri (4.4 per 100,000 in both states); the largest relative and absolute decrease was in Ohio (–20.7%, –6.7). The highest synthetic opioid–involved death rate in 2018 occurred in West Virginia (34.0 per 100,000)." Wilson N, Kariisa M, Seth P, Smith H IV, Davis NL. Drug and Opioid-Involved Overdose Deaths — United States, 2017–2018. MMWR Morb Mortal Wkly Rep 2020;69:290–297. |
| 18. Association of Dose Tapering With Overdose or Mental Health Crisis Among Patients Prescribed Long-term Opioids "In a large cohort of patients in the US prescribed stable, longterm, higher-dose opioids, undergoing opioid dose tapering was associated with statistically significant risk of subsequent overdose and mental health crisis, including suicidality." Agnoli A, Xing G, Tancredi DJ, Magnan E, Jerant A, Fenton JJ. Association of Dose Tapering With Overdose or Mental Health Crisis Among Patients Prescribed Long-term Opioids. JAMA. 2021;326(5):411–419. doi:10.1001/jama.2021.11013 |
| 19. Opioid-Involved Overdose Deaths in the US 2017-2018 "Of the 70,237 drug overdose deaths in the United States in 2017, approximately two thirds (47,600) involved an opioid (1). In recent years, increases in opioid-involved overdose deaths have been driven primarily by deaths involving synthetic opioids other than methadone (hereafter referred to as synthetic opioids) (1). CDC analyzed changes in age-adjusted death rates from 2017 to 2018 involving all opioids and opioid subcategories* by demographic characteristics, county urbanization levels, U.S. Census region, and state. During 2018, a total of 67,367 drug overdose deaths occurred in the United States, a 4.1% decline from 2017; 46,802 (69.5%) involved an opioid (2). From 2017 to 2018, deaths involving all opioids, prescription opioids, and heroin decreased 2%, 13.5%, and 4.1%, respectively. However, deaths involving synthetic opioids increased 10%, likely driven by illicitly manufactured fentanyl (IMF), including fentanyl analogs (1,3)." Wilson N, Kariisa M, Seth P, Smith H 4th, Davis NL. Drug and Opioid-Involved Overdose Deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290‐297. Centers for Disease Control. Published 2020 Mar 20. |
| 20. Drugs Most Frequently Involved in Drug Overdose Deaths in the US 2011–2016 "The percentage of deaths with concomitant involvement of other drugs varied by drug. For example, almost all drug overdose deaths involving alprazolam or diazepam (96%) mentioned involvement of other drugs. In contrast, 50% of the drug overdose deaths involving methamphetamine, and 69% of the drug overdose deaths involving fentanyl mentioned involvement of one or more other specific drugs. "Table D shows the most frequent concomitant drug mentions for each of the top 10 drugs involved in drug overdose deaths in 2016. " Two in five overdose deaths involving cocaine also mentioned fentanyl. " Nearly one-third of drug overdose deaths involving fentanyl also mentioned heroin (32%). " Alprazolam was mentioned in 26% of the overdose deaths involving hydrocodone, 22% of the deaths involving methadone, and 25% of the deaths involving oxycodone. " More than one-third of the overdose deaths involving cocaine also mentioned heroin (34%). " More than 20% of the overdose deaths involving methamphetamine also mentioned heroin." Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. National Vital Statistics Reports; vol 67 no 9. Hyattsville, MD: National Center for Health Statistics. 2018. |
| 21. Drugs Most Frequently Mentioned in Overdose Deaths in the US 2011-2016 "The number of drug overdose deaths per year increased 54%, from 41,340 deaths in 2011 to 63,632 deaths in 2016 (Table A). From the literal text analysis, the percentage of drug overdose deaths mentioning at least one specific drug or substance increased from 73% of the deaths in 2011 to 85% of the deaths in 2016. The percentage of drug overdose deaths that mentioned only a drug class but not a specific drug or substance declined from 5.1% of deaths in 2011 to 2.5% in 2016. Review of the literal text for these deaths indicated that the deaths that mentioned only a drug class frequently involved either an opioid or an opiate (ranging from 54% in 2015 to 60% in 2016). The percentage of deaths that did not mention a specific drug or substance or a drug class declined from 22% of drug overdose deaths in 2011 to 13% in 2016." Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. National Vital Statistics Reports; vol 67 no 9. Hyattsville, MD: National Center for Health Statistics. 2018. |
| 22. Drugs Most Frequently Involved in Drug Overdose Deaths in the US 2011–2016 "For the top 15 drugs: " Among drug overdose deaths that mentioned at least one specific drug, oxycodone ranked first in 2011,heroin from 2012 through 2015, and fentanyl in 2016. " In 2011 and 2012, fentanyl was mentioned in approximately 1,600 drug overdose deaths each year, but mentions increased in 2013 (1,919 deaths),2014 (4,223 deaths), 2015 (8,251 deaths), and 2016(18,335 deaths). In 2016, 29% of all drug overdose deaths mentioned involvement of fentanyl. " The number of drug overdose deaths involving heroin increased threefold, from 4,571 deaths or 11% of all drug overdose deaths in 2011 to 15,961 deaths or 25% of all drug overdose deaths in 2016. " Throughout the study period, cocaine ranked second or third among the top 15 drugs. From 2014 through 2016, the number of drug overdose deaths involving cocaine nearly doubled from 5,892 to 11,316. " The number of drug overdose deaths involving methamphetamine increased 3.6-fold, from 1,887 deaths in 2011 to 6,762 deaths in 2016. " The number of drug overdose deaths involving methadone decreased from 4,545 deaths in 2011 to 3,493 deaths in 2016." Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. National Vital Statistics Reports; vol 67 no 9. Hyattsville, MD: National Center for Health Statistics. 2018. |
| 23. Xylazine is a Kappa-Opioid Agonist with Gender-Specific Responses to Opioid Antagonists (e.g. Naloxone) "Here, we report the first xylazine dose-response locomotor study in male and female mice as well as the first assessment of adrenergic- and opioid-receptor antagonist-precipitated withdrawal symptoms following, xylazine, fentanyl, and xylazine/fentanyl administration in mice. These experiments show that male and female mice are differentially sensitive to xylazine. We find female mice are less sensitive to the motor-suppressing effects of xylazine contrary to the recent findings in rats reported by Khatri et al. (2023), potentially due to their use of repeated dosing of xylazine or species differences [27]. Using a modified version of our 3-day precipitated withdrawal model [40,41,46], we show xylazine is indeed responsive to naloxone, contrary to common assumptions made by both health professionals and in the media [7]. Both sexes exhibited some level of somatic withdrawal behaviors to xylazine and naloxone, though females showed sensitized behavioral responding. Indeed, females appear to be as sensitive, if not more sensitive to xylazine withdrawal than fentanyl withdrawal at tested doses, while males remain much more responsive to fentanyl withdrawal conditions. At the doses tested in our study, the effect of naloxone precipitated withdrawal on xylazine/fentanyl combination was synergistic as compared to each drug in isolation. This was especially apparent when examining increased bouts of paw tremors, which may represent a more passive coping behavior that we have previously observed is sexually dimorphic in opioid withdrawal [41]. In contrast, we did not observe similar findings when withdrawal was precipitated by atipamezole, an α2-AR antagonist used anesthesia reversal in veterinary medicine. These intriguing findings led us to consider the possibility of direct xylazine activity on opioid receptors. Previous studies have shown that xylazine is antinociceptive, results in a cross-tolerance to some mechanisms of opioid induced antinociception, and that these effects are naloxone-sensitive, but surprisingly not sensitive to the κOR selective antagonist nor-BNI [57–60]. Congruent with this data, we did not observe significant expression of withdrawal behavior to nor-BNI precipitated withdrawal, and pretreatment with nor-BNI exacerbated naloxone precipitated withdrawal in female mice. Until now, xylazine was thought to exert these effects through promotion of endogenous opioid release and xylazine has not been directly tested as a potential opioid agonist. We are the first to report definitive evidence that xylazine acts as a full agonist at κOR and is biased towards G-protein signaling pathways." Bedard ML, Huang XP, Murray JG, et al. Xylazine is an agonist at kappa opioid receptors and exhibits sex-specific responses to opioid antagonism. Addict Neurosci. 2024;11:100155. doi:10.1016/j.addicn.2024.100155 |
| 24. Nalmefene vs Naloxone "As shown above, the data supports that these stronger, longer-acting agents may be unnecessary, with other research suggesting their existence may also cause undue harm. Using a stronger or longer-acting antagonist as a one-size-fits-all approach may put patients at greater risk for experiencing more severe and/or prolonged withdrawal symptoms.(Bennett et al., 2020; Hill et al., 2022; Neale & Strang, 2015) Providers may find it difficult to manage withdrawal symptoms and comorbidities like chronic pain, forcing the patient to suffer until the reversal agent wears off. It is also notable to consider how patients who are naïve to nalmefene may react upon discharge following administration. These patients may attempt to self-manage withdrawal symptoms or cravings only to find higher opioid doses are required to overcome the nalmefene blockade, increasing their propensity to overdose as was observed when patients began adjusting to naloxone.(Neale & Strang, 2015) Alternatively, patients accustomed to opioid withdrawal symptoms subsiding within 1 to 2 h after naloxone administration may not be able to tolerate several hours of withdrawal, increasing both the likelihood of attempts to overcome the blockade and resistance to using reversal agents in the future.(Neale & Strang, 2015) Considering the average layperson likely does not fully grasp the potential harm of nalmefene, and that any opioid overdose education they may have received from an opioid overdose education & naloxone distribution (OEND) program would have been naloxone and harm reduction focused, adding these agents into the market creates opportunities for greater clinical complication. This lack of familiarity combined with the lack of clinical discretionary knowledge by the layperson who may be administering these medications in the field sets the stage for nalmefene exposure to elicit prolonged agitation and negative consequences.(Brenner et al., 2021) Furthermore, it is possible that nalmefene administration may complicate the initiation of medications for opioid use disorder such as buprenorphine/naloxone, which can be done in as little as three hours following the last opioid use when co-administered with naloxone.(Randall et al., 2023) Additionally, the FDA approved intranasal naloxone for over-the-counter use in March 2023. It is yet to be seen how this will affect its insurance coverage and medication access.(Harris, 2023b) This may especially affect vulnerable patient populations such as those with limited disposable income. Coverage for prescription nalmefene may serve some relief when naloxone is not covered or attainable by other means." Infante AF, Elmes AT, Gimbar RP, Messmer SE, Neeb C, Jarrett JB. Stronger, longer, better opioid antagonists? Nalmefene is NOT a naloxone replacement. Int J Drug Policy. 2024;124:104323. doi:10.1016/j.drugpo.2024.104323 |
| 25. Xylazine and Overdoses "Xylazine is a non-opiate sedative, analgesic, and muscle relaxant that shares its drug class (α2-adrenoreceptor agonists) with medications such as clonidine, lofexidine, tizanidine, and dexmedetomidine [6]. It was initially developed as an antihypertensive agent by Farbenfabriken Bayer AG in 1962; however, subsequent testing revealed severe adverse events related to hypotension and central nervous system (CNS) depression [6, 7]. Consequently, xylazine never gained approval for human use; however, it was approved by the US Food and Drug Administration (FDA) in 1972 exclusively for use in veterinary medicine [6, 7]. At present, xylazine remains unregulated under both the Controlled Substances Act (CSA) in the USA [8] and the Controlled Drugs and Substances Act (CDSA) in Canada [9]. "Fatal xylazine-positive overdoses, often co-occurring with synthetic compounds such as IMF and its analogs, surged dramatically in the past decade in North America. These overdoses have increased approximately 12-fold between 2018 and 2021 in the USA [6]. Importantly, naloxone—an opioid antagonist medication that is safe and effective for reversing opioid-induced respiratory depression during overdose—does not directly address the effects of xylazine as it is not an opioid, thereby introducing new challenges regarding overdose response best practices within clinical- and community-based settings [8, 10]. Altogether, this pressing issue has prompted The White House Office of National Drug Control Policy (ONDCP) to designate fentanyl associated or adulterated with xylazine (FAAX) as an emergent health threat to the USA in April 2023 and issue a comprehensive response plan in July 2023 [11, 12]. Similar cases are also on the rise in Canada and other countries such as the UK, marking the first xylazine-involved overdose outside of North America [9, 13]. Against the backdrop of this global health crisis, it is imperative to renew efforts in delivering evidence-based public health and harm reduction programs to facilitate secondary and tertiary prevention of adverse health outcomes following xylazine exposure." Zhu DT. Public health impact and harm reduction implications of xylazine-involved overdoses: a narrative review. Harm Reduct J. 2023;20(1):131. Published 2023 Sep 12. doi:10.1186/s12954-023-00867-x |
| 26. Rescue Breathing and Naloxone in Response to Overdose "Relevant literature on overdose response included 3 clinical guidelines,1,21,32 3 grey literature reports (a rapid review,36 an evidence brief37 and a report of a technical working group on resuscitation training38), and a pilot and feasibility study.39 The conclusions in these resources differ on overdose response, notably on the role of rescue breathing and the order in which resuscitation steps occur. An in-depth discussion of the literature is available in Appendix 1, and Appendix 3 contains more detail on findings and included studies. "As the mandate of THN [Take Home Naloxone] programs includes overdose response training, our recommendation focuses on trained overdose response. Evidence from the Naloxone Guidance Development Group indicates that community overdose responders are effectively trained through different methods. For the purposes of this document, we recognize that people using THN programs may be trained on overdose response through their peers, using online resources, THN programs or cardiopulmonary resuscitation (CPR) training courses. "In the literature, multiple sources identified naloxone administration and calling 911 or other emergency response numbers as critical steps in overdose response.1,21,32,36,38,39 Three guidance documents included verbal and physical stimulation to assess whether someone is experiencing overdose and to stimulate breathing.21,32,38 "For a responder trained in overdose response, guidance may differ according to whether the responder suspects respiratory depression or cardiac arrest. Overdose response must take the pathophysiology of opioid overdose into account. When someone experiences opioid overdose, regulation of breathing is impaired, respiration is depressed and insufficient oxygen reaches the brain and other organs.1 Because the person experiencing overdose is not breathing effectively, oxygen also cannot reach the heart and the individual may experience cardiac arrest (i.e., their heart stops beating or beats too ineffectively to support their vital organs).1" Ferguson M, Rittenbach K, Leece P, et al. Guidance on take-home naloxone distribution and use by community overdose responders in Canada. CMAJ. 2023;195(33):E1112-E1123. doi:10.1503/cmaj.230128 |
| 27. Rescue Breathing in Response to Overdose "Rescue breathing for persons suspected of having an opioid overdose has considerable support among harm reduction programs and in the medical literature.18 This preference is based on the physiology of an opioid overdose. Opioids suppress the autonomic respiratory response to declining oxygen saturation and rising carbon dioxide levels. If this response remains suppressed, the consequences are hypoxia, acidosis, organ failure and death. The majority, if not all, of the community-based naloxone programs in the United States train responders in a rescue breathing technique. In this technique, the nostrils of the unconscious individual are pinched closed, a seal is formed between the mouths of the victim and the responder, and breaths are introduced every five seconds by the responder. Further support for rescue breathing comes from the Substance Abuse and Mental Health Services Administration (SAMHSA) in its Opioid Overdose Toolkit.19 In late 2014, WHO issued guidelines on community management of opioid overdose recommending, 'In suspected opioid overdose, first responders should focus on airway management, assisting ventilation and administering naloxone.'20 This was rated as a strong recommendation based on a weak quality of evidence." New York State Technical Working Group on Resuscitation Training in Naloxone Provision Programs: 2016 Report. New York State, Department of Health, AIDS Institute; 2016:16. |
| 28. Involvement of Fentanyl in Overdose Deaths in the US "Fentanyl was detected in 56.3% of 5,152 opioid overdose deaths in the 10 states during July–December 2016 (Figure). Among these 2,903 fentanyl-positive deaths, fentanyl was determined to be a cause of death by the medical examiner or coroner in nearly all (97.1%) of the deaths. Northeastern states (Maine, Massachusetts, New Hampshire, and Rhode Island) and Missouri** reported the highest percentages of opioid overdose deaths involving fentanyl (approximately 60%–90%), followed by Midwestern and Southern states (Ohio, West Virginia, and Wisconsin), where approximately 30%–55% of decedents tested positive for fentanyl. New Mexico and Oklahoma reported the lowest percentage of fentanyl-involved deaths (approximately 15%–25%). In contrast, states detecting any fentanyl analogs in >10% of opioid overdose deaths were spread across the Northeast (Maine, 28.6%, New Hampshire, 12.2%), Midwest (Ohio, 26.0%), and South (West Virginia, 20.1%) (Figure) (Table 1). "Fentanyl analogs were present in 720 (14.0%) opioid overdose deaths, with the most common being carfentanil (389 deaths, 7.6%), furanylfentanyl (182, 3.5%), and acetylfentanyl (147, 2.9%) (Table 1). Fentanyl analogs contributed to death in 535 of the 573 (93.4%) decedents. Cause of death was not available for fentanyl analogs in 147 deaths.†† Five or more deaths involving carfentanil occurred in two states (Ohio and West Virginia), furanylfentanyl in five states (Maine, Massachusetts, Ohio, West Virginia, and Wisconsin), and acetylfentanyl in seven states (Maine, Massachusetts, New Hampshire, New Mexico, Ohio, West Virginia, and Wisconsin). U-47700 was present in 0.8% of deaths and found in five or more deaths only in Ohio, West Virginia, and Wisconsin (Table 1). Demographic characteristics of decedents were similar among overdose deaths involving fentanyl analogs and fentanyl (Table 2). Most were male (71.7% fentanyl and 72.2% fentanyl analogs), non-Hispanic white (81.3% fentanyl and 83.6% fentanyl analogs), and aged 25–44 years (58.4% fentanyl and 60.0% fentanyl analogs) (Table 2). "Other illicit drugs co-occurred in 57.0% and 51.3% of deaths involving fentanyl and fentanyl analogs, respectively, with cocaine and confirmed or suspected heroin detected in a substantial percentage of deaths (Table 2). Nearly half (45.8%) of deaths involving fentanyl analogs tested positive for two or more analogs or fentanyl, or both. Specifically, 30.9%, 51.1%, and 97.3% of deaths involving carfentanil, furanylfentanyl, and acetylfentanyl, respectively, tested positive for fentanyl or additional fentanyl analogs. Forensic investigations found evidence of injection drug use in 46.8% and 42.1% of overdose deaths involving fentanyl and fentanyl analogs, respectively. Approximately one in five deaths involving fentanyl and fentanyl analogs had no evidence of injection drug use but did have evidence of other routes of administration. Among these deaths, snorting (52.4% fentanyl and 68.8% fentanyl analogs) and ingestion (38.2% fentanyl and 29.7% fentanyl analogs) were most common. Although rare, transdermal administration was found among deaths involving fentanyl (1.2%), likely indicating pharmaceutical fentanyl (Table 2). More than one third of deaths had no evidence of route of administration." Julie K. O’Donnell, PhD; John Halpin, MD; Christine L. Mattson, PhD; Bruce A. Goldberger, PhD; R. Matthew Gladden, PhD. Deaths Involving Fentanyl, Fentanyl Analogs, and U-47700 — 10 States, July–December 2016. Morbidity and Mortality Weekly Report. Vol. 66. Centers for Disease Control. October 27, 2017. |
| 29. American College of Medical Toxicology and the American Academy of Clinical Toxicology position statement: nalmefene should not replace naloxone as the primary opioid antidote at this time "As physicians, pharmacists, scientists, and specialists in poison information, we are experts in pharmacology, toxicology, and the management of opioid overdose and addiction. We applaud the effort to seek out new therapeutic strategies for the management of these patients. "We are concerned that the use of a longer-acting reversal agent would not improve on current practice and could potentially cause harm. When withdrawal is precipitated by an opioid antagonist, there are few good management options. In most cases, the best strategy is to address and support the patient’s signs and symptoms until the effects of the antagonist wane. In the case of naloxone, which has a relatively short duration of action, severe withdrawal usually lasts less than an hour with symptoms typically persisting no more than 90 min [Citation25–27]. A longer-acting antagonist is anticipated to cause longer-lasting precipitated withdrawal and may lead to worse patient outcomes. Clinical experience with both naltrexone and nalmefene suggests prolonged withdrawal is a complication of longer-acting opioid antagonists [Citation28]. Although a longer-acting antagonist may be theoretically beneficial for the resuscitation of opioid-naive individuals in an opioid-induced mass casualty incident, this type of event has never been reported in North America and this application is unstudied. "We are also concerned that patients who receive nalmefene may require longer periods of observation, by up to several hours, to observe for recrudescent effects as the antagonist effects wane. Patients who receive nalmefene will still need medical observation to ensure that respiratory depression does not recur after the effects of the medication subside. This will prolong emergency department visit length and challenge patient and clinician expectations, further burdening a taxed system. Further clinical study is needed to understand whether a reduction in repeat antagonist use justifies a longer length of stay or longer period of withdrawal. "Finally, we are concerned that intranasal nalmefene has not been adequately studied for effectiveness in the actual setting and patient population: for patients with severe opioid intoxication in the out-of-hospital environment. Lack of proof of safety and efficacy in real-world use could result in significant harm if widely utilized. "The potential benefits of nalmefene over naloxone (greater opioid receptor affinity, longer duration action) carry the risk of causing harm. These benefits, if present, should be demonstrated in the clinical environment, balanced with the risks, and compared to naloxone prior to the broad adoption of nalmefene." Andrew I. Stolbach, Maryann E. Mazer-Amirshahi, Lewis S. Nelson & Jon B. Cole (2023) American College of Medical Toxicology and the American Academy of Clinical Toxicology position statement: nalmefene should not replace naloxone as the primary opioid antidote at this time, Clinical Toxicology, 61:11, 952-955, DOI: 10.1080/15563650.2023.2283391 |
| 30. Naloxone vs Nalmefene "While the addition of stronger, longer-acting opioid overdose reversal agents expands the options available to combat the fatal opioid overdose crisis, their inception is perhaps without clinical grounds. Data supports continued practice without these stronger, longer acting nalmefene agents, and it is unclear whether any benefits nalmefene offers outweigh the apparent risks of its use. Nalmefene may yet find a clinical niche, but at this time, appears to be a solution designed to resolve hypothetical complications without fully understanding the unintended consequences of use. As such, without further evidence healthcare professionals should not support the use of stronger, longer-acting opioid overdose reversal agents. Further study is necessary, before nalmefene, or other naloxone alternatives should be incorporated into general practice." Infante AF, Elmes AT, Gimbar RP, Messmer SE, Neeb C, Jarrett JB. Stronger, longer, better opioid antagonists? Nalmefene is NOT a naloxone replacement. Int J Drug Policy. 2024;124:104323. doi:10.1016/j.drugpo.2024.104323 |
| 31. Association of Dose Tapering With Overdose or Mental Health Crisis "In the current study, tapering was associated with absolute differences in rates of overdose or mental health crisis events of approximately 3 to 4 events per 100 person-years compared with nontapering. These findings suggest that adverse events associated with tapering may be relatively common and support HHS recommendations for more gradual dose reductions when feasible and careful monitoring for withdrawal, substance use, and psychological distress.9 "Previous research has examined adverse outcomes associated with discontinuing long-term opioids.10-14 This analysis demonstrated associations between adverse outcomes and a more sensitive indicator of opioid dose reduction (≥15% from baseline). The associations persisted in sensitivity analyses that excluded patients who discontinued opioids during follow-up, suggesting that the observed associations between tapering and overdose and mental health crisis are not entirely explained by events occurring in patients discontinuing opioids. Additionally, all categories of maximum dose reduction velocity demonstrated higher relative rates of outcomes compared with the lowest (<10% per month), suggesting that risks were not confined to patients undergoing rapid tapering. "Patients undergoing tapering from higher baseline opioid doses had higher associated risk for the study outcomes compared with patients undergoing tapering from lower baseline doses. Due to physiologic opioid tolerance,27 patients receiving higher doses may have heightened intolerance of opioid dose disruption, potentially warranting additional caution in patients tapering from higher doses." Agnoli A, Xing G, Tancredi DJ, Magnan E, Jerant A, Fenton JJ. Association of Dose Tapering With Overdose or Mental Health Crisis Among Patients Prescribed Long-term Opioids. JAMA. 2021;326(5):411–419. doi:10.1001/jama.2021.11013 |
| 32. Safe Supply and Non-Fatal Overdose "In this study involving 47 individuals who were admitted to an unsanctioned compassion club, we found that enrolment in the program was associated with a reduction in any type of non-fatal overdose as well as non-fatal overdose involving naloxone administration. These findings, suggesting that enrollment in DULF's intervention likely decreased overdose rates, appear to be amongst the first in a growing body of research on the impacts of a safer drug supply that does not employ the medical system. "Our findings are aligned with previous evaluations of safer supply programs that have found positive outcomes associated with program engagement, as well as the findings of the scoping review of safer supply programs published in this issue (Ledlie et al. 2024). A previous quantitative study investigating a medicalized and prescriber-based model of safer supply found that enrolment in such programming reduced use of emergency departments, hospital admissions and healthcare costs (Gomes et al., 2022). In addition, several qualitative investigations of safer supply programs, involving prescriber- and vending machine-based programs, have found that such programs help reduce illicit drug use, overdose risk, and led to other improvements in health, social and financial well-being (Bardwell, Ivsins, Mansoor, Nolan, & Kerr, 2023; Ivsins, Boyd, Beletsky, & McNeil, 2020; Ivsins, Boyd, Mayer, et al., 2020; Ivsins et al., 2021; Ledlie et al. 2024; Schmidt et al., 2023). Perhaps most relevant to the current study, a recent quantitative study of a prescriber-based opioid safer supply program in Toronto reported an 80% reduction in non-fatal overdose among participants after 8 months of program engagement (Nefah et al, 2023). However, such programs are known to often suffer from low enrolment and retention rates, attributed in part to inability of such programs to accommodate a large number of individuals and a lack of desirable options and dose for people who use drugs (May, Holloway, Buhociu, & Hills, 2020). This problem may be further compounded by the medical system's inability to prescribe or allow access to illegal drugs (Tyndall, 2020). This in turn has prompted calls for the implementation of more community-based compassion club models operating outside of the medical system as a means of increasing access to safer supply (Thomson et al., 2019). Indeed, some physician leaders have expressed that they would rather not to be responsible for ensuring access to safer supply given the associated ethical issues and the current state of the overburdened healthcare system (Bach, 2022). Our study contributes to the existing literature by describing the impact of a non-medicalized safer supply program on non-fatal overdose. "People who use drugs, and other experts in the field, have long expressed a demand for a stable, predictable, and easy to access supply of drugs to prevent overdose in the context of the current overdose crisis (Bonn et al., 2020; Health Canada, 2023a; BC Coroners Service, 2023a; Tyndall, 2020). Despite its limited scope, this study has implications for research and policy development specific to safer supply and overdose prevention. The lack of active studies in the field of de-medicalized safer supply distribution highlights the need for more research. Given the recent arrest of DULF's co-founders (Greer, 2023), pathways for exemptions to Canada's Controlled Drugs and Substances Act are needed to enable institutions to run programs and track relevant statistics that can assist policymakers in making decisions (Bonn et al., 2021), as well as revisions to existing policy frameworks, specifically the Special Access Program, the Controlled Drugs and Substances Act, and Food and Drugs Act, which limit the implementation of compassion clubs as a response to Canada's public health crisis (Bonn et al., 2021). This policy hurdle is further compounded by a lack of available licit substances for such a program; there are currently no appropriate approved drugs in Canada's Drug Product Database (Health Canada, 2023b). This further underscores the need for policy changes that facilitate a deeper understanding of the effectiveness of compassion clubs as a means of optimizing support for individuals who are at risk of overdose. Further, additional prospective study of effectiveness is needed, alongside qualitative studies focused on implementation issues and cost-effectiveness research to further uncover the impacts and limitations of this unique approach to safe supply programming." Jeremy Kalicum, Eris Nyx, Mary Clare Kennedy, Thomas Kerr, The impact of an unsanctioned compassion club on non-fatal overdose, International Journal of Drug Policy, 2024, 104330, ISSN 0955-3959, doi.org/10.1016/j.drugpo.2024.104330. |
| 33. Polydrug Involvement in Pharmaceutical Overdose Deaths in the US "Opioids were frequently implicated in overdose deaths involving other pharmaceuticals. They were involved in the majority of deaths involving benzodiazepines (77.2%), antiepileptic and antiparkinsonism drugs (65.5%), antipsychotic and neuroleptic drugs (58.0%), antidepressants (57.6%), other analgesics, antipyretics, and antirheumatics (56.5%), and other psychotropic drugs (54.2%). Among overdose deaths due to psychotherapeutic and central nervous system pharmaceuticals, the proportion involving only a single class of such drugs was highest for opioids (4903/16 651; 29.4%) and lowest for benzodiazepines (239/6497; 3.7%)." Christopher M. Jones, PharmD, Karin A. Mack, PhD, and Leonard J. Paulozzi, MD, "Pharmaceutical Overdose Deaths, United States, 2010," Journal of the American Medical Association, February 20, 2013, Vol 309, No. 7, p. 658. |
| 34. Growth of Xylazine in US Drug Market "We summarize longitudinal, recent, and geographically specific evidence describing how xylazine is increasingly implicated in overdose deaths in jurisdictions spanning all major US regions and link it to detailed ethnographic observations of its use in Philadelphia open-air narcotics markets. Xylazine presence in overdose deaths grew exponentially during the observed period, rising nearly 20-fold between 2015 and 2020. Whereas the most recent national data from the State Unintentional Drug Overdose Reporting System characterized the level of xylazine-present overdoses in 2019 (Kariisa, 2021), we found that the prevalence increased by nearly 50% from 2019 to 2020 alone, indicating a need for more recent data to guide the public health response. Furthermore, we find that even looking at only 10 jurisdictions a greater number of xylazine-present overdose deaths were seen in 2020 (854), than the previous study looking at 38 states in 2019 (826) (Kariisa, 2021), implying a very fast rate of growth nationally. "Xylazine prevalence was observed earliest and at the highest magnitude in the Northeast, and may be spreading west, in a pattern similar to the trajectory of illicitly-manufactured fentanyls in recent years (Shover et al., 2020). This similarity may not be incidental, as an analysis of the co-occurrence of fentanyl and xylazine indicates a strong ecological link, with fentanyl nearly universally implicated in xylazine-present overdose deaths. Further, ethnographic data among PWID suggests that the use of xylazine as an illicit drug additive may predominantly serve as a response to the short duration of fentanyl. By ‘giving fentanyl legs’—offering improved duration of effect—the addition of xylazine may confer a competitive market advantage for illicit opioid formulations that contain it, as it remedies one of the most commonly expressed complaints that PWID hold regarding fentanyl-based street opioid formulations." Friedman, J., Montero, F., Bourgois, P., Wahbi, R., Dye, D., Goodman-Meza, D., & Shover, C. (2022). Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug and alcohol dependence, 233, 109380. doi.org/10.1016/j.drugalcdep.2022.109380. |
| 35. Xylazine-Involved Deaths "Xylazine, an alpha-2 receptor agonist, is used in veterinary medicine as a sedative and muscle relaxant; it is not approved for use in humans. However, reports of adulteration of illicit opioids with xylazine have been increasing in the United States (1–3). In humans, xylazine can cause respiratory depression, bradycardia, and hypotension (4). Typical doses of naloxone are not expected to reverse the effects of xylazine; therefore, persons who use xylazine-adulterated opioids are at high-risk for fatal overdose. Although some regions of the United States have reported increases in xylazine-involved deaths, xylazine was involved in <2% of overdose deaths nationally in 2019 (2,5). Most xylazine-involved deaths are associated with fentanyls, including fentanyl analogs (1,5)." Chhabra, N., Mir, M., Hua, M. J., Berg, S., Nowinski-Konchak, J., Aks, S., Arunkumar, P., & Hinami, K. (2022). Notes From the Field: Xylazine-Related Deaths - Cook County, Illinois, 2017-2021. MMWR. Morbidity and mortality weekly report, 71(13), 503–504. doi.org/10.15585/mmwr.mm7113a3 |
| 36. Changes Demographics, Number, and Substance Involved in Drug Overdoses in the US 1979-2016 "The overall mortality rate for unintentional drug poisonings in the United States grew exponentially from 1979 through 2016. This exponentially increasing mortality rate has tracked along a remarkably smooth trajectory (log linear R2 = 0.99) for at least 38 years (left panel). By contrast, the trajectories of mortality rates from individual drugs have not tracked along exponential trajectories. Cocaine was a leading cause in 2005–2006, which was overtaken successively by prescription opioids, then heroin, and then synthetic opioids such as fentanyl. The demographic patterns of deaths due to each drug have also shown substantial variability over time. Until 2010, most deaths were in 40- to 50-year old persons, from cocaine and increasingly from prescription drugs. Deaths from heroin and then fentanyl have subsequently predominated, affecting younger persons, ages 20 to 40 (middle panel). Mortality rates for males have exceeded those for females for all drugs. Rates for whites exceeded those for blacks for all opioids, but rates were much greater among blacks for cocaine. Death rates for prescription drugs were greater for rural than urban populations. The geographic patterns of deaths also vary by drug. Prescription opioid deaths are widespread across the United States (right panel), whereas heroin and fentanyl deaths are predominantly located in the northeastern United States and methamphetamine deaths in the southwestern United States. Cocaine deaths tend to be associated with urban centers." Hawre Jalal, et al. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science, Sept. 21, 2018. Vol. 361, Issue 6408, eaau1184. DOI: 10.1126/science.aau1184. |
| 37. Take-Home Naloxone Does Not Lead To Riskier Drug Use "We did not find evidence that THN [Take-Home Naloxone] training was associated with risk compensation behavior in this cohort of people who inject drugs. Rather, there was no significant change in frequency of injecting any drugs, injecting opioids, or using benzodiazepines after accessing THN. There was also no change in the proportion of time that participants reported using drugs alone, a key indicator of overdose mortality risk.30,38,39 "There was no evidence of THN-associated compensatory risk behavior in this cohort. While not all overdose risk behaviors were examined in this study (eg, injecting in public, concomitant use of alcohol or benzodiazepines, and use of fentanyl),40,41 frequency of opioid injecting and frequency of benzodiazepine use are 2 of the most important risk factors for overdose. The association between knowledge of and engagement in overdose risk behaviors is complex,38 and THN is designed to be used on other people who may be at risk of overdose; therefore, it may be pertinent to examine the implications of naloxone availability for drug use in peer networks. In a qualitative study, participants with opioid use disorder residing in residential drug treatment programs in the US described both no change to their drug use and some engagement in riskier behavior by themselves or peers (eg, injecting heroin laced with fentanyl).42 However, this finding has not been borne out in empirical evidence and does not appear to correspond with increases in overdose at the population level.3,4 "Findings from this work are consistent with an emerging evidence base suggesting that concerns about risk compensation with naloxone availability are unfounded.4 Yet, these concerns continue to be raised as objections for expanding THN supply.7,11 For example, a number of pharmacists in a recent Australian study expressed concerns about distributing naloxone, as they believed that recipients would feel comfortable increasing their opioid use.43 However, because naloxone administration can be associated with opioid withdrawal and reverses the effects of any opioids that have been recently taken, the outcomes of naloxone are considered unpleasant by people who inject drugs, meaning that they are typically reluctant to administer the drug.42,44 Furthermore, it is questionable whether this concern is reason enough to withhold a lifesaving medication from people. Only 40.4% of participants in the SuperMIX study reported THN training, despite most of the sample reporting the use of opioids. There is a clear need for widespread education among health care practitioners and other key stakeholders to enable them to address this common assumption about THN, which can act as a barrier to THN supply so that coverage is increased." Colledge-Frisby S, Rathnayake K, Nielsen S, et al. Injection Drug Use Frequency Before and After Take-Home Naloxone Training. JAMA Netw Open. 2023;6(8):e2327319. doi:10.1001/jamanetworkopen.2023.27319 |
| 38. Rising Levels Of Stimulant Overdose Mortality In The US "Of the 1,220,143 deaths with involved drugs listed on the death certificate, 130 560 (10.7% of all decedents) were found to have stimulants listed. Among stimulant-involved deaths, 93,689 decedents (71.8%) were men, the median (interquartile range) age was 45 (34-54) years, and 98,635 (75.5%) were White (Table). Of these, 120,803 certificates (92.5%) listed only illicit stimulants, 5544 (4.2%) listed only medical stimulants, and 3524 listed both types (2.7%). Among illicit stimulants, there were 77,013 deaths (61.9%) involving cocaine, 49,602 deaths (39.9%) involving methamphetamine, and 817 deaths (0.7%) involving 3,4-methylenedioxymethamphetamine. Among medical stimulants, there were 8240 deaths (90.9%) involving amphetamine, 295 deaths (0.3%) involving methylphenidate, and 615 deaths (0.7%) involving pseudoephedrine. Among all 3 stimulant groups, the proportion of deaths that also involved opioids was substantial; concomittant use of benzodiazepines and antidepressants was also not uncommon. "Stimulant mortality has risen rapidly since 2010 (Figure). The mortality rate involving all stimulants rose from 2.913 deaths per 100,000 population in 2010 to 9.690 in 2017. Mortality rates increased among all medical stimulants (ARR, 1.226; 95% CI, 1.202-1.250), amphetamine (ARR, 1.118; 95% CI, 1.082-1.155), cocaine (ARR, 1.234;95% CI, 1.222-1.245), and methamphetamine (ARR, 1.278; 95% CI, 1.261-1.295)." Black JC, Bau GE, Iwanicki JL, Dart RC. Association of Medical Stimulants With Mortality in the US From 2010 to 2017. JAMA Intern Med. Published online February 01, 2021. |
| 39. Good Samaritan and Naloxone Access Laws Save Lives "GAO found that 48 jurisdictions (47 states and D.C.) have enacted both Good Samaritan and Naloxone Access laws. Kansas, Texas and Wyoming do not have a Good Samaritan law for drug overdoses but have a Naloxone Access law. The five U.S. territories do not have either type of law. GAO also found that the laws vary. For example, Good Samaritan laws vary in the types of drug offenses that are exempt from prosecution and whether this immunity takes effect before an individual is arrested or charged, or after these events but before trial. "GAO reviewed 17 studies that provide potential insights into the effectiveness of Good Samaritan laws in reducing overdose deaths or the factors that may contribute to a law’s effectiveness. GAO found that, despite some limitations, the findings collectively suggest a pattern of lower rates of opioid-related overdose deaths among states that have enacted Good Samaritan laws, both compared to death rates prior to a law’s enactment and death rates in states without such laws. In addition, studies found an increased likelihood of individuals calling 911 if they are aware of the laws. However, findings also suggest that awareness of Good Samaritan laws may vary substantially across jurisdictions among both law enforcement officers and the public, which could affect their willingness to call 911." "Most States Have Good Samaritan Laws and Research Indicates They May Have Positive Effects," US General Accountability Office, March 2021, GAO-21-248. |
| 40. Deaths from Drug Overdose in the United States in 2015 "During 2015, drug overdoses accounted for 52,404 U.S. deaths, including 33,091 (63.1%) that involved an opioid. There has been progress in preventing methadone deaths, and death rates declined by 9.1%. However, rates of deaths involving other opioids, specifically heroin and synthetic opioids other than methadone (likely driven primarily by illicitly manufactured fentanyl) (2,3), increased sharply overall and across many states." Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–1452. |
| 41. Xylazine-Involved and Xylazine-Associated Deaths in Cook County, IL "A xylazine-associated death was defined as a positive postmortem xylazine serum toxicology test result in an unintentional, undetermined, or pending intent substance-related death during January 2017–October 2021. Routine postmortem tests were conducted for other substances including fentanyl, fentanyl analogs, cocaine, and naloxone. Xylazine testing is standard in Cook County for suspected drug overdose deaths. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.* "A total of 236 xylazine-associated deaths were reported during the study period. Xylazine-associated deaths increased throughout the study period; incidence peaked during July 2021 (Figure). The percentage of fentanyl-associated deaths involving xylazine also increased throughout the study period, rising to a peak of 11.4% of fentanyl-related deaths assessed by the Cook County Medical Examiner’s Office during October 2021. Fentanyl or fentanyl analogs were detected on forensic testing in most xylazine-involved deaths (99.2%). Other common co-occurring substances included diphenhydramine (79.7%), cocaine (41.1%), and quinine (37.3%). Naloxone was detected in 32.2% of xylazine-associated deaths." Chhabra, N., Mir, M., Hua, M. J., Berg, S., Nowinski-Konchak, J., Aks, S., Arunkumar, P., & Hinami, K. (2022). Notes From the Field: Xylazine-Related Deaths - Cook County, Illinois, 2017-2021. MMWR. Morbidity and mortality weekly report, 71(13), 503–504. doi.org/10.15585/mmwr.mm7113a3 |
| 42. Receipt of Opioid Use Disorder Treatments Prior to Fatal Overdoses and Comparison to No Treatment "The findings revealed that exposures to MOUD, even if not continued throughout the six-month exposure period was associated with reduced risk of a fatal poisoning compared to non-MOUD forms of treatment and no treatment exposure. It is also clear that risk of death associated with exposure to non-MOUD forms of treatment was no less than that for no treatment; indeed, non-MOUD treatment might have produced worse outcomes than no treatment. Comparing the relative risk for the treatments for which agency-based numbers are available revealed that any exposure to methadone in the six months prior to death in 2017 was associated with 65% reduced relative risk of fatal opioid poisoning compared to exposure to any non-MOUD treatment recorded in the DMHAS database. Even more apparent, based on the available data from 2017, the relative risk of fatal opioid death in the six months following exposure to non-MOUD treatments ranged from 1.5 to 1.74 compared to no treatment. This is an unacceptably high probability for treatments that are purported to benefit patients with OUD and likely to be paid for by public tax revenues. In fact, it seems likely, based on our estimates of the number of people with OUD not exposed to treatment, that non-MOUD treatments were inferior to no treatment. "There is a century of data demonstrating that non-MOUD treatment is followed by a high rate of relapse to opioid use – especially for morphine and heroin – approaching 90% at six months (Musto, 1999, Broers et al., 2000, Heimer et al., 2019). Relapse rates for those regularly using fentanyl may be even higher (Stone et al. 2018). There is ample evidence from the U.S. and elsewhere that longer-term non-MOUD treatments place those who relapse at an especially high risk of opioid overdose and death.(Strang, Beswick and Gossop, 2003; Wakeman et al. 2020). There is also compelling evidence that agonist MOUD decreases opioid-involved and all-cause mortality (Santo et al. 2021), and nearly thirty years of evidence that methadone reduces HIV-related mortality (Fugelstad et al., 1995, Parashar et al., 2016, Sordo et al., 2017). Our analysis was based on exposures to treatment, not their completion or retention, therefore our findings indicate that exposures to agonist MOUD treatment convey more benefit that non-MOUD even if the treatment is incompletely adhered to or terminated." Robert Heimer, Anne C. Black, Hsiuju Lin, Lauretta E. Grau, David A. Fiellin, Benjamin A. Howell, Kathryn Hawk, Gail D’Onofrio, William C. Becker, Receipt of Opioid Use Disorder Treatments Prior to Fatal Overdoses and Comparison to No Treatment in Connecticut, 2016-17, Drug and Alcohol Dependence, 2023, 111040, ISSN 0376-8716, doi.org/10.1016/j.drugalcdep.2023.111040. |
| 43. Prescription Opioid Tapering, Overdose Risk, and Suicidality "In this emulated trial including more than 400 000 episodes of stable long-term opioid therapy, opioid tapering was associated with a small (0.15%) absolute increase in the risk of overdose or suicide events compared with a stable dosage during 11 months of follow-up. We did not identify a difference in the risk of overdose or suicide events between abrupt discontinuation and stable dosage, although the smaller number of episodes categorized as abrupt discontinuation may have reduced precision. The findings were robust to secondary and sensitivity analyses. "The risk ratio of 1.15 for opioid overdose or suicide events associated with opioid tapering was smaller than in past studies conducted in other populations. This study examined commercially insured individuals receiving a stable long-term opioid dosage without evidence of opioid misuse. A large study of Veterans Health Administration patients estimated adjusted hazard ratios between 1.7 and 6.8 for the association of treatment discontinuation with suicide or overdose among patient subgroups defined by length of prior treatment.17 A study of Oregon Medicaid recipients found adjusted hazard ratios for suicide of 3.6 for discontinuation and 4.5 for tapering.18 A study using the same claims data set and similar definition of long-term opioid therapy as our study identified effect estimates between those in our study and those in prior studies, with an estimated adjusted incidence rate ratio of 1.3 for the association of dose tapering with overdose and 2.4 for the association of dose tapering with suicide attempts.32" Larochelle MR, Lodi S, Yan S, Clothier BA, Goldsmith ES, Bohnert ASB. Comparative Effectiveness of Opioid Tapering or Abrupt Discontinuation vs No Dosage Change for Opioid Overdose or Suicide for Patients Receiving Stable Long-term Opioid Therapy. JAMA Netw Open. 2022;5(8):e2226523. doi:10.1001/jamanetworkopen.2022.26523 |
| 44. Trends in Drug Overdose Mortality in the US 2000-2019 "The number of accidental drug overdose deaths increased by 622% between 2000 and 2020, and age-standardized mortality rates increased nearly four-fold in both men and women. Age-period-cohort decomposition found rapid increases in mortality since 2012 in men and women, with higher mortality risk in cohorts born after 1990. The fastest increase occurred in Black Americans since 2012, and Americans of all races born after 1975 had significantly higher mortality risk, with mortality risk increasing rapidly in more recent cohorts. The peak of mortality has shifted from the 40–59 age group to the 30–40 year age group in the past decade." Fujita-Imazu, S., Xie, J., Dhungel, B., Wang, X., Wang, Y., Nguyen, P., Khin Maung Soe, J., Li, J., & Gilmour, S. (2023). Evolving trends in drug overdose mortality in the USA from 2000 to 2020: an age-period-cohort analysis. EClinicalMedicine, 61, 102079. doi.org/10.1016/j.eclinm.2023.102079 |
| 45. Deaths in the UK Due to a Toxic Drug Supply and Drug Overdose "In 2020 drug related deaths in the United Kingdom (UK) reached the highest rate in over 25 years (ONS, 2021). Data between 2001-2018 evidences a substantial increase in drug poisonings over time for people who use opioids, with risk increasing particularly between the years of 2010-2018, an effect which was not entirely explained by the ageing of this cohort (Lewer et al., 2022). The concentration of drug related deaths are geographically varied in the UK. Areas of high economic deprivation, such as North-East England have more than three times the rate of drug related deaths than London (ONS, 2021). In the North East town of Middlesbrough citizens are statistically more likely to die from a drug related deaths than a car accident (Middlesbrough Council, 2020). Poverty, homelessness, an aging population of opioid users, unemployment, polydrug use and significant funding reductions for drug treatment services have been posited as contributing factors (ACMD, 2017; Lewer et al., 2022; ONS, 2019a, 2019b; Public Health England, 2018). The largest proportion of drug related deaths in the North-East of England are reported among men who are dependent on illicit opioids, such as heroin (ONS, 2022). The high prevalence of opioid usage in Middlesbrough combined with an unregulated and toxic illicit street tablet market (substances such as z-drugs, benzodiazepine and gabapentinoids) provides a potentially fatal risk environment due to interactions between these depressant drugs, which can significantly increase risk of drug related deaths (Akhgari, Sardari-Iravani, & Ghadipasha, 2021; Ford & Law, 2014; ONS, 2021, 2022)." Poulter, H. L., Walker, T., Ahmed, D., Moore, H. J., Riley, F., Towl, G., & Harris, M. (2023). More than just 'free heroin': Caring whilst navigating constraint in the delivery of diamorphine assisted treatment. The International journal on drug policy, 116, 104025. doi.org/10.1016/j.drugpo.2023.104025 |
| 46. Growing Involvement of Xylazine in Deaths Due to a Toxic Drug Supply and Overdose "In overdose data from 10 jurisdictions – representing all four major US census regions – xylazine was found to be increasingly present in overdose mortality (Fig. 1). The highest prevalence was observed in Philadelphia, (with xylazine present in 25.8% of overdose deaths in 2020), followed by Maryland (19.3% in 2021) and Connecticut (10.2% in 2020). In 2021, xylazine prevalence also grew substantially in Jefferson County, Alabama, reaching 8.4% of overdose fatalities. Across the four census regions, the Northeast had the highest prevalence, and the West had the lowest (Fig. 2), with only six xylazine-present overdose deaths in total detected in Phoenix, Arizona, and 1 in San Diego County, California. Across jurisdictions, a clear increasing trend was noted. Pooling data for 2015, a total xylazine prevalence of 0.36% was observed. By 2020, this had grown to 6.7% of overdose deaths, representing a 20-fold increase. From 2019–2020 – the last year of data available for all jurisdictions – the prevalence increased by 44.8%." Friedman, J., Montero, F., Bourgois, P., Wahbi, R., Dye, D., Goodman-Meza, D., & Shover, C. (2022). Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug and alcohol dependence, 233, 109380. doi.org/10.1016/j.drugalcdep.2022.109380. |
| 47. Law Enforcement Disruption of Drug Markets and Overdose "Our population-based study provides evidence that police seizures of substances identified as opioids or stimulants are significantly associated with increased spatiotemporal clustering of overdose events in the immediate surrounding geographic area (radii of 100 m, 250 m, and 500 m) over 1-, 2-, and 3-week periods. Importantly, the difference in spatiotemporal clustering of all 3 overdose event rates before and after opioid-related seizures was higher than expected under the estimated null distribution across all radii and time intervals although this pattern of association was less consistent among stimulant-related seizures. This is consistent with our hypothesized mechanism because persons with opioid use disorder who lose their supply will experience both diminishing tolerance and withdrawal, whereby even the anticipation of painful symptoms may lead them to seek a new supply while discounting risks that stem from the differences in potency inherent in an illicit opioid market; this results in unknown tolerance, uncertainty about a safe dose, and increased overdose risk."We were unable to assert a causal relationship between law enforcement drug market disruptions and overdose, and our study was not designed to, but our results are consistent with other evidence of this association.18,19,22–24 Moreover, federal agencies already recognize the harms that emerge from these disruptions; for example, the Centers for Disease Control and Prevention developed the Opioid Rapid Response Program, an interagency effort designed to reduce overdose by rapidly increasing access to treatment of chronic pain and substance use disorder in the wake of enforcement actions against pain clinics and opioid prescribers.25,26 Routine supply-side interdictions among police may merit similar efforts to prevent resulting overdose in the surrounding community—but with more frequent need, given the prevailing volume of seizures."Officers might also use the considerable discretion at their disposal when interacting with persons who use drugs, particularly in enforcing misdemeanors or nonviolent felonies that regulate drugs to reduce harms that might come from disrupting an individual’s drug supply.27 Additionally, our study suggests that information on drug seizures may provide a touchpoint that is further upstream than other postoverdose events, providing greater potential to mitigate harms. For example, although the role of law enforcement in overdose remains a topic of debate,28 public safety partnerships could entail timely notice of interdiction events to agencies that provide overdose prevention services, outreach, and referral to care.25" Ray, B., Korzeniewski, S. J., Mohler, G., Carroll, J. J., Del Pozo, B., Victor, G., Huynh, P., & Hedden, B. J. (2023). Spatiotemporal Analysis Exploring the Effect of Law Enforcement Drug Market Disruptions on Overdose, Indianapolis, Indiana, 2020-2021. American journal of public health, 113(7), 750–758. doi.org/10.2105/AJPH.2023.307291 |
| 48. Association of Opioid Overdose Laws with Opioid Use and Mortality " Naloxone access laws that ease restrictions on naloxone possession and distribution are associated with a 20% reduction overdose deaths among African-Americans. " Good Samaritan laws, providing immunity from prosecution for those calling emergency services, are associated with broad reductions in overdose deaths, reducing overdose deaths by 13% overall. " None of these harm reduction measures result in increase in opioid or heroin use. " These laws are effective at reducing overdose mortality without creating additional opioid use. Correspondingly, these measures should be considered an important part of the strategy used to address the opioid epidemic." McClellan, Chandler, Lambdin, Barrot H., et al. Opioid-overdose laws association with opioid use and overdose mortality. Addictive Behaviors. March 19, 2018. |
| 49. Criminalization Does More Harm Than Good "Our study adds to a growing body of literature that suggests drug criminalization and supply-side interdiction might produce more public harm than public good. This casts doubt on the core assumption of state and federal drug policy and suggests that police officers intending to protect the public’s health and safety may be inadvertently exacerbating harms such as fatal overdose. Policymakers need to revisit the role drug policies play in perpetuating an overdose epidemic that is negatively affecting the nation’s life expectancy. This should include careful consideration of the population-level consequences from decades of interdiction efforts that have not resulted in any meaningful reduction in the price or availability of drugs in the community over any substantial period and may contribute to increased risk of overdose and its sequelae, including death." Ray, B., Korzeniewski, S. J., Mohler, G., Carroll, J. J., Del Pozo, B., Victor, G., Huynh, P., & Hedden, B. J. (2023). Spatiotemporal Analysis Exploring the Effect of Law Enforcement Drug Market Disruptions on Overdose, Indianapolis, Indiana, 2020-2021. American journal of public health, 113(7), 750–758. doi.org/10.2105/AJPH.2023.307291 |
| 50. Deaths in the US Due to Overdose and/or Toxic Drug Supply 1999-2004 "The number of unintentional poisoning deaths increased from 12,186 in 1999 to 20,950 in 2004. The annual age-adjusted rate increased 62.5%, from 4.4 per 100,000 population in 1999 to 7.1 in 2004. The increase among females, from 2.3 to 4.7 per 100,000 population (103.0%), was twice the increase among males, from 6.5 to 9.5 per 100,000 population (47.1%) (Table 1). Among males, rates among whites, American Indians/Alaska Natives, and Asians/Pacific Islanders all increased approximately 50%. Rates among black males were highest in 1999 but did not increase. Among females, rates among whites more than doubled, whereas nonwhites had smaller increases or decreased. Overall, rates increased 75.8% among whites, 55.8% among American Indians/Alaska Natives, 27.4% among Asians/Pacific Islanders, and 11.2% among blacks. Rates among non-Hispanics increased more than rates among Hispanics for both sexes. Among all sex and racial/ethnic groups, the largest increase (136.5%) was among non-Hispanic white females. Among all age groups, the largest increase occurred among persons aged 15--24 years (113.3%). In 2004, the highest rates were among persons aged 35--54 years, who accounted for 59.6% of all poisoning deaths that year. "From 1999 to 2004, rates increased by less than one third in the Northeast and West but more than doubled in the South and nearly doubled in the Midwest.† Delaware, Maryland, New York, and Rhode Island had decreases in rates, and California had the smallest increase (4.0%) (Figure). States with the largest relative increases were West Virginia (550%), Oklahoma (226%), Maine (210%), Montana (195%), and Arkansas (195%). Increases of 100% or more occurred in 23 states: 11.8% (two of 17) of states§ in the most urban tertile, 41.2% (seven of 17) of those in the middle tertile, and 82.4% (14 of 17) of those in the most rural tertile (extended Mantel-Haenszel chi-square for linear trend across the tertiles = 15.4, p<0.001). "The increase in poisoning mortality occurred almost exclusively among persons whose deaths were coded as unintentional drug poisoning (X40--X44), for which the rate increased 68.3% (Table 2). The rate for poisoning deaths attributed to other substances (X45--X49) increased 1.3%. By 2004, drug poisoning accounted for 19,838 deaths, 94.7% of all unintentional poisoning deaths. Among types of drug poisoning, the greatest increases were in the "other and unspecified" drug, psychotherapeutic drug, and "narcotic and hallucinogen" drug categories." Centers for Disease Control and Prevention (CDC) (2007). Unintentional poisoning deaths--United States, 1999-2004. MMWR. Morbidity and mortality weekly report, 56(5), 93–96. |
| 51. Use of Cannabis as a Response to the Overdose Crisis "The opioid epidemic is a public health crisis that is at least partially driven by harms associated with POM [Prescription Opioid Medication] use. States are passing laws allowing use of MC [Medical Cannabis] and patients are using MC, but currently there is little understanding of how this influences POM use or of MC-related harms. This literature review provides preliminary evidence that states with MC laws have experienced reported decreases in POM use, abuse, overdose, and costs. However, existing evidence is limited by significant methodological shortcomings; so, general conclusions are difficult to draw. "The use of MC as an alternative to POMs for pain management warrants additional empirical attention as a potential harm reduction strategy. NASEM (2017) recommends more clinical trials to elucidate appropriate MC forms, routes of administration, and combination of products for treating pain, but access to MC products to fully evaluate these questions is challenging due to federal regulations. However, the recently funded National Institutes of Health longitudinal study to research the impacts of MC on opioid use is a critical step in the right direction (National Institute of Health, 2017, Williams, 2017). MCs potential as an alternative pain treatment modality to help mitigate the major public health opioid crisis, could be a missed opportunity if data on safety, efficacy, and outcomes are not collected and explored. Health care practitioners, particularly nurses who are charged with ensuring patient comfort, have a vested interest in providing viable alternatives to POMs when appropriate, as part of an integrative approach to pain management, and must advocate for more research to better understand the public health implications and risks and benefits of such alternatives." Vyas, Marianne Beare et al. The use of cannabis in response to the opioid crisis: A review of the literature. Nursing Outlook, January-February 2018, Volume 66, Issue 1, 56 - 65. |
| 52. Treatment with Methadone or Buprenorphine Following Nonfatal Overdose Leads to Decreased Mortality "In the 12 months after a nonfatal overdose, 2040 persons (11%) enrolled in MMT for a median of 5 months (interquartile range, 2 to 9 months), 3022 persons (17%) received buprenorphine for a median of 4 months (interquartile range, 2 to 8 months), and 1099 persons (6%) received naltrexone for a median of 1 month (interquartile range, 1 to 2 months). Among the entire cohort, all-cause mortality was 4.7 deaths (95% CI, 4.4 to 5.0 deaths) per 100 person-years and opioid-related mortality was 2.1 deaths (CI, 1.9 to 2.4 deaths) per 100 person-years. Compared with no MOUD, MMT was associated with decreased all-cause mortality (adjusted hazard ratio [AHR], 0.47 [CI, 0.32 to 0.71]) and opioid-related mortality (AHR, 0.41 [CI, 0.24 to 0.70]). Buprenorphine was associated with decreased all-cause mortality (AHR, 0.63 [CI, 0.46 to 0.87]) and opioid-related mortality (AHR, 0.62 [CI, 0.41 to 0.92]). No associations between naltrexone and all-cause mortality (AHR, 1.44 [CI, 0.84 to 2.46]) or opioid-related mortality (AHR, 1.42 [CI, 0.73 to 2.79]) were identified." Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Annals of Internal Medicine. Epub ahead of print 19 June 2018. doi: 10.7326/M17-3107. |
| 53. The DOPE SRO Project "In 2021, the SFDPH [San Francisco Department of Public Health]/DOPE [Drug Overdose Prevention & Education] Project collaboration initiated a pilot program designed to reduce fatal overdoses in permanent supportive SROs by mobilizing and supporting tenant overdose response within these buildings. Known as the DOPE SRO Project, this program recruited, trained, and compensated tenants to serve as overdose prevention specialists (hereafter referred to as 'specialists') who help prevent overdose deaths in the building through naloxone distribution and peer-to-peer training in overdose identification and response. The program was piloted in two supportive housing sites that have experienced escalating overdose death. The first site is a large SRO (160 units) located in the Tenderloin neighborhood that has been operating for over four decades and is home to a mix of long-term and recently housed tenants. The second site is a smaller SRO (50 units) located in the South of Market Street (SoMa) that has been operational since 2018. Both buildings offer case management services and other supports (e.g. food programs, community programming) to tenants, who are referred through the city's Coordinated Entry Systems for homelessness services (Department of Homelessness and Supportive Housing 2022)." Michelle Olding, Neena Joshi, Stacy Castellanos, Emily Valadao, Lauren Hall, Laura Guzman, Kelly Knight, Saving lives in our homes: Qualitative evaluation of a tenant overdose response program in supportive, single-room occupancy (SRO) housing, International Journal of Drug Policy, Volume 118, 2023, 104084, ISSN 0955-3959, doi.org/10.1016/j.drugpo.2023.104084. |
| 54. Opioid-overdose laws association with opioid use and overdose mortality "Results "Conclusions McClellan, C., Lambdin, B. H., Ali, M. M., Mutter, R., Davis, C. S., Wheeler, E., Pemberton, M., & Kral, A. H. (2018). Opioid-overdose laws association with opioid use and overdose mortality. Addictive behaviors, 86, 90–95. doi.org/10.1016/j.addbeh.2018.03.014. |
| 55. Tenant-Led Naloxone Distribution and Overdose Education in SRO Settings "Our findings contribute further evidence supporting tenant-led naloxone distribution and overdose education as a critical intervention to address overdose vulnerability in SRO [Single Room Occupancy] settings (Bardwell et al., 2019; Nowell & Masuda, 2020). At the time of writing, the City of San Francisco funds naloxone distribution in seven of its approximately 75 supportive housing SROS, and has committed to making naloxone available in all its supportive housing facilities by 2026 (San Francisco Department of Public Health 2022; Thadani & Palomino, 2022). Rapidly increasing naloxone availability is crucial to reducing overdose deaths in SROs (Bardwell et al., 2017; Rowe et al., 2019). This evaluation foregrounds the benefits of pairing targeted naloxone distribution with programs that train and compensate tenants to lead overdose education and response in their buildings. The city has so far earmarked $1 million dollars to expand the SRO program model into eight supportive housing facilities (San Francisco Department of Public Health 2022). This investment is promising and will allow the specialist program to run in eight additional SROs until June 2023. However, this evaluation highlights the need for enhanced training and psychosocial supports for the housing staff and tenants who are routinely responding to overdoses. Given the broader forms of support and mutual aid that specialists described in this evaluation, they could benefit from expanded training in other social competencies such as collaborative leadership, crisis response, violence prevention, and conflict de-escalation. Involving tenants early on in program planning and training curriculum development may help better tailor training to needs of different SRO environments. Psychosocial supports including grief counseling and post-overdose de-briefing were also requested by specialists and supportive housing team members to address the emotional burden of overdose response work. Regular check-ins with specialists about their workloads will continue to be important to identify and mitigate scope creep." Michelle Olding, Neena Joshi, Stacy Castellanos, Emily Valadao, Lauren Hall, Laura Guzman, Kelly Knight, Saving lives in our homes: Qualitative evaluation of a tenant overdose response program in supportive, single-room occupancy (SRO) housing, International Journal of Drug Policy, Volume 118, 2023, 104084, ISSN 0955-3959, doi.org/10.1016/j.drugpo.2023.104084. |
| 56. Drug Overdose Deaths in the US Involving Cocaine and Psychostimulants On the Rise "Deaths involving cocaine and psychostimulants have increased in the United States in recent years; among 70,237 drug overdose deaths in 2017, nearly a third (23,139 [32.9%]) involved cocaine, psychostimulants, or both. From 2016 to 2017, death rates involving cocaine and psychostimulants each increased by approximately one third, and increases occurred across all demographic groups, Census regions, and in several states. In 2017, nearly three fourths of cocaine-involved and roughly one half of psychostimulant-involved overdose deaths, respectively, involved at least one opioid. After initially peaking in 2006, trends in overall cocaine-involved death rates declined through 2012, when they began to rise again. The 2006–2012 decrease paralleled a decline in cocaine supply coupled with an increase in cost. Similar patterns in death rates involving both cocaine and opioids were observed, with increases for cocaine- and synthetic opioid-involved deaths occurring from 2012 to 2017. From 2010 to 2017, increasing rates of deaths involving psychostimulants occurred and persisted even in the absence of opioids." Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential — United States, 2003–2017. MMWR Morb Mortal Wkly Rep 2019;68:388–395. |
| 57. Vivitrol and Risk of Opioid Overdose According To The Manufacturer "Vulnerability to Opioid Overdose "After opioid detoxification, patients are likely to have reduced tolerance to opioids. VIVITROL blocks the effects of exogenous opioids for approximately 28 days after administration. However, as the blockade wanes and eventually dissipates completely, patients who have been treated with VIVITROL may respond to lower doses of opioids than previously used, just as they would have shortly after completing detoxification. This could result in potentially life-threatening opioid intoxication (respiratory compromise or arrest, circulatory collapse, etc.) if the patient uses previously tolerated doses of opioids. Cases of opioid overdose with fatal outcomes have been reported in patients who used opioids at the end of a dosing interval, after missing a scheduled dose, or after discontinuing treatment. "Patients should be alerted that they may be more sensitive to opioids, even at lower doses, after VIVITROL treatment is discontinued, especially at the end of a dosing interval (i.e., near the end of the month that VIVITROL was administered), or after a dose of VIVITROL is missed. It is important that patients inform family members and the people closest to the patient of this increased sensitivity to opioids and the risk of overdose [see Patient Counseling Information (17)]. "There is also the possibility that a patient who is treated with VIVITROL could overcome the opioid blockade effect of VIVITROL. Although VIVITROL is a potent antagonist with a prolonged pharmacological effect, the blockade produced by VIVITROL is surmountable. The plasma concentration of exogenous opioids attained immediately following their acute administration may be sufficient to overcome the competitive receptor blockade. This poses a potential risk to individuals who attempt, on their own, to overcome the blockade by administering large amounts of exogenous opioids. Any attempt by a patient to overcome the antagonism by taking opioids is especially dangerous and may lead to life-threatening opioid intoxication or fatal overdose. Patients should be told of the serious consequences of trying to overcome the opioid blockade [see Patient Counseling Information (17)]." Full Prescribing Information. Vivitrol (Naltrexone for Extended-Release Injectable Suspension). Alkermes. Revised December 2015. |
| 58. Overdose Risk Based on Prescription Type "Dunn et al4 found that risk of drug-related adverse events among individuals treated for chronic noncancer pain with opioids was increased at opioid doses equivalent to 50 mg/d or more of morphine. Our analyses similarly found that the risk of opioid overdose increased when opioid dose was equivalent to 50 mg/d or more of morphine. "The present study also extended prior research in several important ways. We used a large, national sample of individuals and focused exclusively on opioid overdose deaths. Because the circumstances that lead to overdose death may vary by the condition for which the opioid is prescribed and substance use disorder status, we conducted analyses for subgroups of patients, including those with cancer, acute pain, and substance use disorders. "The present study also extended the prior research by exploring a novel risk factor, ie, concurrent prescriptions of regularly scheduled and as-needed opioids. We found that those patients who were simultaneously treated with as-needed and regularly scheduled opioids, a strategy for treating pain exacerbations,7,8 did not have a statistically significant increased risk of opioid overdose in adjusted models. Recent treatment guidelines have indicated that the long-term safety of this strategy for pain exacerbation has not been established,5,9 and in the present study we did not find evidence of greater overdose risk associated with this treatment practice after accounting for maximum daily dose and patient characteristics." Bohnert ASB, Valenstein M, Bair MJ, et al. Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths. JAMA. 2011;305(13):1315–1321. doi:10.1001/jama.2011.370 |
| 59. Factors That May Skew Estimates of Overdose Deaths Attributed to Specific Drugs, Particularly Opioids "First, factors related to death investigation might affect rate estimates involving specific drugs. At autopsy, the substances tested for, and circumstances under which tests are performed to determine which drugs are present, might vary by jurisdiction and over time. Second, the percentage of deaths with specific drugs identified on the death certificate varies by jurisdiction and over time. Nationally, 19% (in 2014) and 17% (in 2015) of drug overdose death certificates did not include the specific types of drugs involved. Additionally, the percentage of drug overdose deaths with specific drugs identified on the death certificate varies widely by state, ranging from 47.4% to 99%. Variations in reporting across states prevent comparison of rates between states. Third, improvements in testing and reporting of specific drugs might have contributed to some observed increases in opioid-involved death rates. Fourth, because heroin and morphine are metabolized similarly (9), some heroin deaths might have been misclassified as morphine deaths, resulting in underreporting of heroin deaths. Finally the state-specific analyses of opioid deaths are restricted to 28 states, limiting generalizability." Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–1452. |
| 60. Prescribing Patterns and Opioid Overdose-Related Deaths "There is some evidence that higher prescribed doses increase the risk of drug overdose among individuals treated with opioids for chronic non-cancer pain.4 Specifically, the risk of drug-related adverse events is higher among individuals prescribed opioids at doses equal to 50 mg/d or more of morphine. The association of opioid prescribing patterns with risk of over-dose may vary across groups of patients; opioid treatment recommendations for pain are typically specific to particular subgroups such as those with chronic noncancer pain,5 cancer-related pain, and substance use disorders.6 However, potential subgroup differences in opioid prescribing have not been examined." Bohnert ASB, Valenstein M, Bair MJ, et al. Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths. JAMA. 2011;305(13):1315–1321. doi:10.1001/jama.2011.370 |
| 61. Opioid Toxicity or Overdose "The main toxic effect is decreased respiratory rate and depth, which can progress to apnea. Other complications (eg, pulmonary edema, which usually develops within minutes to a few hours after opioid overdose) and death result primarily from hypoxia. Pupils are miotic. Delirium, hypotension, bradycardia, decreased body temperature, and urinary retention may also occur. "Normeperidine, a metabolite of meperidine, accumulates with repeated use (including therapeutic); it stimulates the central nervous system and may cause seizure activity. "Serotonin syndrome occasionally occurs when fentanyl, meperidine, tramadol, methadone, codeine, or oxycodone is taken concomitantly with other drugs that have serotonergic effects (eg, selective serotonin reuptake inhibitors, monoamine oxidase inhibitors). Serotonin syndrome consists of one or more of the following: "Hypertonia Gerald F. O’Malley, DO, and Rika O’Malley, MD, Opioid Toxicity and Withdrawal, in Merck Manual Professional Version, last accessed August 31, 2021. |
| 62. Heroin Toxicity, Adulterants, and Overdose Potential "If it is not pure drugs that kill, but impure drugs and the mixture of drugs, then the myth of the heroin overdose can be dangerous. If users had a guaranteed pure supply of heroin which they relied on, there would be little more likelihood of toxic doses than occur with narcotics administered in a hospital. "But when people take whatever they can off the street, they have no way of knowing how the drug is adulterated. And when they decide to augment heroin's effects, possibly because they do not want to take too much heroin, they may place themselves in the greatest danger." Peele, Stanton, MD, (1998), The persistent, dangerous myth of heroin overdose. Last accessed August 31, 2021. |
| 63. Lower Opioid Overdose Mortality Rates In States With Medical Cannabis Laws "Although the mean annual opioid analgesic overdose mortality rate was lower in states with medical cannabis laws compared with states without such laws, the findings of our secondary analyses deserve further consideration. State-specific characteristics, such as trends in attitudes or health behaviors, may explain variation in medical cannabis laws and opioid analgesic overdose mortality, and we found some evidence that differences in these characteristics contributed to our findings. When including state-specific linear time trends in regression models, which are used to adjust for hard-to-measure confounders that change over time, the association between laws and opioid analgesic overdose mortality weakened. In contrast, we did not find evidence that states that passed medical cannabis laws had different overdose mortality rates in years prior to law passage, providing a temporal link between laws and changes in opioid analgesic overdose mortality. In addition, we did not find evidence that laws were associated with differences in mortality rates for unrelated conditions (heart disease and septicemia), suggesting that differences in opioid analgesic overdose mortality cannot be explained by broader changes in health. In summary, although we found a lower mean annual rate of opioid analgesic mortality in states with medical cannabis laws, a direct causal link cannot be established." Bacchuber, Marcus A., MD; Saloner, Brendan, PhD; Cunningham, Chinazo O., MD, MS; and Barry, Colleen L., PhD, MPP. "Medical Cannabis Laws and Opioid Analgesic Overdose Mortality in the United States, 1999-2010." JAMA Intern Med. Published online August 25, 2014. |
| 64. Alcohol Overdose
"Abdominal pain. "Home Care "Place the person on their side in case they throw up (vomit). DO NOT make the person throw up unless told to do so by a health care professional or Poison Control. "Check the person frequently to make sure their condition does not get worse. "If the person is not alert (unconscious) or only somewhat alert (semi-conscious), emergency assistance may be needed. When in doubt, call for medical help." Ethanol Poisoning, MEDLINEplus Medical Encyclopedia, US National Library of Medicine, last accessed August 31, 2021. |
| 65. Methamphetamine Overdose "Tachycardia, arrhythmias, chest pain, hypertension, dizziness, nausea, vomiting, and diarrhea can occur. Central nervous system effects include acute delirium and toxic psychosis. Overdose can also cause stroke (usually hemorrhagic), seizures, muscle rigidity, and hyperthermia (>40° C); all of these effects may precipitate rhabdomyolysis, which can lead to renal failure." Gerald F. O’Malley, DO, and Rika O’Malley , MD, Amphetamines (Methamphetamines), in Merck Manual Professional Version, last accessed August 31, 2021. |
| 66. Overdose Risk Based on Prescription Type "Dunn et al4 found that risk of drug-related adverse events among individuals treated for chronic noncancer pain with opioids was increased at opioid doses equivalent to 50 mg/d or more of morphine. Our analyses similarly found that the risk of opioid overdose increased when opioid dose was equivalent to 50 mg/d or more of morphine. "The present study also extended prior research in several important ways. We used a large, national sample of individuals and focused exclusively on opioid overdose deaths. Because the circumstances that lead to overdose death may vary by the condition for which the opioid is prescribed and substance use disorder status, we conducted analyses for subgroups of patients, including those with cancer, acute pain, and substance use disorders. "The present study also extended the prior research by exploring a novel risk factor, ie, concurrent prescriptions of regularly scheduled and as-needed opioids. We found that those patients who were simultaneously treated with as-needed and regularly scheduled opioids, a strategy for treating pain exacerbations,7,8 did not have a statistically significant increased risk of opioid overdose in adjusted models. Recent treatment guidelines have indicated that the long-term safety of this strategy for pain exacerbation has not been established,5,9 and in the present study we did not find evidence of greater overdose risk associated with this treatment practice after accounting for maximum daily dose and patient characteristics." Bohnert ASB, Valenstein M, Bair MJ, et al. Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths. JAMA. 2011;305(13):1315–1321. doi:10.1001/jama.2011.370 |
| 67. Cannabis Overdose: Toxic Dosage and Mortality Risk "Tetrahydrocannabinol is a very safe drug. Laboratory animals (rats, mice, dogs, monkeys) can tolerate doses of up to 1,000 mg/kg (milligrams per kilogram). This would be equivalent to a 70 kg person swallowing 70 grams of the drug—about 5,000 times more than is required to produce a high. Despite the widespread illicit use of cannabis there are very few if any instances of people dying from an overdose. In Britain, official government statistics listed five deaths from cannabis in the period 1993-1995 but on closer examination these proved to have been deaths due to inhalation of vomit that could not be directly attributed to cannabis (House of Lords Report, 1998). By comparison with other commonly used recreational drugs these statistics are impressive." Iversen, Leslie L., PhD, FRS, "The Science of Marijuana" (London, England: Oxford University Press, 2000), p. 178, citing House of Lords, Select Committee on Science and Technology, "Cannabis — The Scientific and Medical Evidence" (London, England: The Stationery Office, Parliament, 1998). |
| 68. Alcohol Overdose "In alcohol-naïve people, a BAC of 300 to 400 mg/dL (65.1 to 86.8 mmol/L) often causes unconsciousness, and a BAC ≥ 400 mg/dL( 86.8 mmol/L) may be fatal. Sudden death due to respiratory depression or arrhythmias may occur, especially when large quantities are drunk rapidly. This problem is emerging in US colleges but has been known in other countries where it is more common. Other common effects include hypotension and hypoglycemia. "The effect of a particular BAC varies widely; some chronic drinkers seem unaffected and appear to function normally with a BAC in the 300 to 400 mg/dL (65.1 to 86.8 mmol/L) range, whereas nondrinkers and social drinkers are impaired at a BAC that is inconsequential in chronic drinkers." Gerald F. O’Malley, DO, and Rika O’Malley, MD, Alcohol Toxicity and Withdrawal, in Merck Manual Professional Version, last accessed August 31, 2021. |
| 69. Growth in Number of Prescription Drug Overdoses 2004-2009 "In 2009, 1.2 million emergency department (ED) visits (an increase of 98.4% since 2004) were related to misuse or abuse of pharmaceuticals, compared with 1.0 million ED visits related to use of illicit drugs such as heroin and cocaine (3)." Centers for Disease Control and Prevention, Vital Signs: Overdoses of Prescription Opioid Pain Relievers — United States, 1999–2008, Morbidity and Mortality Weekly Report, November 4, 2011 / 60(43);1487-1492 |
| 70. Prescription Opioid Overdose "Among patients who are prescribed opioids, an estimated 80% are prescribed low doses (<100 mg morphine equivalent dose per day) by a single practitioner (7,8), and these patients account for an estimated 20% of all prescription drug overdoses (Figure 3). Another 10% of patients are prescribed high doses (?100 mg morphine equivalent dose per day) of opioids by single prescribers and account for an estimated 40% of prescription opioid overdoses (9,10). The remaining 10% of patients are of greatest concern. These are patients who seek care from multiple doctors and are prescribed high daily doses, and account for another 40% of opioid overdoses (11). Persons in this third group not only are at high risk for overdose themselves but are likely diverting or providing drugs to others who are using them without prescriptions. In fact, 76% of nonmedical users report getting drugs that had been prescribed to someone else, and only 20% report that they acquired the drug from their own doctor (4). Furthermore, among persons who died of opioid overdoses, a significant proportion did not have a prescription in their records for the opioid that killed them; in West Virginia, Utah, and Ohio, 25%–66% of those who died of pharmaceutical overdoses used opioids originally prescribed to someone else (11–13). These data suggest that prevention of opioid overdose deaths should focus on strategies that target 1) high-dosage medical users and 2) persons who seek care from multiple doctors, receive high doses, and likely are involved in drug diversion." Centers for Disease Control, CDC Grand Rounds: Prescription Drug Overdoses — a U.S. Epidemic, Morbidity and Mortality Weekly Report, January 13, 2012 / 61(01);10-13 |
| 71. Heroin Toxicity and Opiate Overdose "A striking finding from the toxicological data was the relatively small number of subjects in whom morphine only was detected. Most died with more drugs than heroin alone 'on board', with alcohol detected in 45% of subjects and benzodiazepines in just over a quarter. Both of these drugs act as central nervous system depressants and can enhance and prolong the depressant effects of heroin." Zador, Deborah, Sunjic, Sandra, and Darke, Shane, Heroin-related deaths in New South Wales, 1992: toxicological findings and circumstances, The Medical Journal of Australia, 1996; 164 (4): 204-207. |
| 72. Treatment for Amphetamine Overdose "When significant oral toxicity is recent (eg, < 1 to 2 h), activated charcoal may be given to limit absorption, although this intervention has not been shown to reduce morbidity or mortality. Urinary acidification hastens amphetamine excretion, but it may worsen myoglobin precipitation in the renal tubules and thus is not recommended. "Benzodiazepines are the preferred initial treatment for CNS excitation, seizures, tachycardia, and hypertension. Lorazepam 2 to 3 mg IV q 5 min titrated to effect may be used. High doses or a continuous infusion may be required. Propofol, with mechanical ventilation, may be required for severe agitation. Hypertension that does not respond to benzodiazepines is treated with nitrates (occasionally nitroprusside or other antihypertensives as needed, depending on the severity of the hypertension. ?-Blockers (eg, metoprolol 2 to 5 mg IV) may be used for severe ventricular arrhythmias or tachycardia. "Hyperthermia can be life threatening and should be managed aggressively with sedation plus evaporative cooling, ice packs, and maintenance of intravascular volume and urine flow with IV normal saline solution." Gerald F. O’Malley, DO, and Rika O’Malley , MD, Amphetamines (Methamphetamines), in Merck Manual Professional Version, last accessed August 31, 2021. |
| 73. Overdose Prevention a Priority "A first priority for prevention must be to reduce the frequency of drug overdoses. We should inform heroin users about the risks of combining heroin with alcohol and other depressant drugs. Not all users will act on such information, but if there are similar behavioral changes to those that occurred with needle-sharing overdose deaths could be substantially reduced. Heroin users should also be discouraged from injecting alone and thereby denying themselves assistance in the event of an overdose." Wayne D. Hall, PhD, "How can we reduce heroin 'overdose' deaths?" The Medical Journal of Australia (MJA 1996; 164:197). |
| 74. Alcohol Poisoning Deaths in the US "On average, 6 people died every day from alcohol poisoning in the US from 2010 to 2012. Alcohol poisoning is caused by drinking large quantities of alcohol in a short period of time. Very high levels of alcohol in the body can shutdown critical areas of the brain that control breathing, heart rate, and body temperature, resulting in death. Alcohol poisoning deaths affect people of all ages but are most common among middle-aged adults and men." "Alcohol Poisoning Deaths: A deadly consequence of binge drinking," CDC Vital Signs, January 2015. |
| 75. Overdose - Opiates "The disadvantage of continuing to describe heroin-related fatalities as 'overdoses' is that it attributes the cause of death solely to heroin and detracts attention from the contribution of other drugs to the cause of death. Heroin users need to be educated about the potentially dangerous practice of concurrent polydrug and heroin use." Zador, Deborah, Sunjic, Sandra, and Darke, Shane, Heroin-related deaths in New South Wales, 1992: toxicological findings and circumstances, The Medical Journal of Australia, 1996; 164 (4): 204-207. |
| 76. Effects of Amphetamine and Methamphetamine Use "A paranoid psychosis may result from long-term use; rarely, the psychosis is precipitated by a single high dose or by repeated moderate doses. Typical features include delusions of persecution, ideas of reference (notions that everyday occurrences have special meaning or significance personally meant for or directed to the patient), and feelings of omnipotence. Some users experience a prolonged depression, during which suicide is possible. Recovery from even prolonged amphetamine psychosis is usual but is slow. The more florid symptoms fade within a few days or weeks, but some confusion, memory loss, and delusional ideas commonly persist for months." Gerald F. O’Malley, DO, and Rika O’Malley , MD, Amphetamines (Methamphetamines), in Merck Manual Professional Version, last accessed August 31, 2021. |
| 77. Factors Influencing Methadone-Related Mortality "Still, methadone is a potent drug; fatal overdoses have been reported over the years (Baden, 1970; Gardner, 1970; Clark, et al., 1995; Drummer, et al., 1992). As with most other opioids, the primary toxic effect of excessive methadone is respiratory depression and hypoxia, sometimes accompanied by pulmonary edema and/or aspiration pneumonia (White and Irvine, 1999; Harding-Pink, 1993). Among patients in addiction treatment, the largest proportion of methadone-associated deaths have occurred during the drug's induction phase, usually when (1) treatment personnel overestimate a patient's degree of tolerance to opioids, or (2) a patient uses opioids or other central nervous system (CNS) depressant drugs in addition to the prescribed methadone (Karch and Stephens, 2000; Caplehorn, 1998; Harding-Pink, 1991; Davoli, et al., 1993). In fact, when deaths occur during later stages of treatment, other drugs usually are detected at postmortem examination (Appel, et al., 2000). In particular, researchers have called attention to the 'poison cocktail' resulting from the intake of multiple psychotropic drugs (Borron, et al., 2001; Haberman, et al., 1995) such as alcohol, benzodiazepines, and other opioids. When used alone, many of these substances are relatively moderate respiratory depressants; however, when combined with methadone, their additive or synergistic effects can be lethal (Kramer, 2003; Payte and Zweben, 1998). Center for Substance Abuse Treatment, Methadone-Associated Mortality: Report of a National Assessment, May 8-9, 2003. SAMHSA Publication No. 04-3904. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, 2004. |
| 78. Cocaine Toxicity or Overdose "An overdose may cause severe anxiety, panic, agitation, aggression, sleeplessness, hallucinations, paranoid delusions, impaired judgment, tremors, seizures, and delirium. Mydriasis and diaphoresis are apparent, and heart rate and blood pressure are increased. Death may result from myocardial infarction or arrhythmias. "Severe overdose causes a syndrome of acute psychosis (eg, schizophrenic-like symptoms), hypertension, hyperthermia, rhabdomyolysis, coagulopathy, renal failure, and seizures. Patients with extreme clinical toxicity may, on a genetic basis, have decreased (atypical) serum cholinesterase, an enzyme needed for clearance of cocaine. "Patients who inhale cocaine may develop an acute pulmonary syndrome (crack lung) with fever, hemoptysis, and hypoxia, that may progress to respiratory failure. "The concurrent use of cocaine and alcohol produces a condensation product, cocaethylene, which has stimulant properties and may contribute to toxicity." Gerald F. O’Malley, DO, and Rika O’Malley , MD, Cocaine (Crack), in Merck Manual Professional Version, last accessed August 31, 2021. |
| 79. Naloxone As Lifesaving Intervention To Prevent Death By Opioid Overdose "The heart of the challenge is the possibility that things could be different: overdose is a public health problem that can be solved. Unlike many of the other leading causes of death, death from opioid overdose is almost entirely preventable,21 and preventable at a low cost.22 Opioids kill by depressing respiration, a slow mode of death that leaves plenty of time for effective medical intervention.23 Overdose is rapidly reversed by the administration of a safe and inexpensive drug called naloxone. Naloxone strips clean the brain’s opioid receptors and reverses the respiratory depression causing almost immediate withdrawal.24 A growing number of harm reduction organizations in the United States are offering overdose prevention programs that provide injection drug users with resuscitation training and take-home doses of naloxone.25" Burris, Scott; Beletsky, Leo; Castagna, Carolyn; Coyle, Casey; Crowe, Colin; and McLaughlin, Jennie Maura, "Stopping an Invisible Epidemic: Legal Issues in the Provision of Naloxone to Prevent Opioid Overdose," Drexel Law Review, Philadelphia, PA: Earle Mack School of Law, Spring 2009, Vol. 1, Number 2. |
| 80. Need for User Education on Overdose Prevention and Harm Reduction "Our findings that an ambulance was called while the subject was still alive in only 10% of cases, and that a substantial minority of heroin users died alone, strongly suggest that education campaigns should also emphasise that it is safer to inject heroin in the company of others, and important to call for an ambulance early in the event of an overdose. Consideration should also be given to trialling the distribution of the opioid antagonist naloxone to users to reduce mortality from heroin use." Zador, Deborah, Sunjic, Sandra, and Darke, Shane, "Heroin-related deaths in New South Wales, 1992: toxicological findings and circumstances," The Medical Journal of Australia, 1996; 164 (4): 204-207. |
| 81. Feasibility of Naloxone Distribution to People Who Use Injection Drugs "This pilot trial is the first in North America to prospectively evaluate a program of naloxone distribution to IDUs [Injection Drug Users] to prevent heroin overdose death. After an 8-hour training, our study participants' knowledge of heroin overdose prevention and management increased, and they reported successful resuscitations during 20 heroin overdose events. All victims were reported to have been unresponsive, cyanotic, or not breathing, but all survived. These findings suggest that IDUs can be trained to respond to heroin overdose by using CPR and naloxone, as others have reported. Moreover, we found no evidence of increases in drug use or heroin overdose in study participants. These data corroborate the findings of several feasibility studies recommending the prescription and distribution of naloxone to drug users to prevent fatal heroin overdose." Seal, Karen H., Robert Thawley, Lauren Gee, Joshua Bamberger, Alex H. Kral, Dan Ciccarone, Moher Downing, and Brian R. Edlin, "Naloxone Distribution and Cardiopulmonary Resuscitation Training for Injection Drug Users to Prevent Heroin Overdose Death: A Pilot Intervention Study," Journal of Urban Medicine, New York, NY: New York Academy of Medicine, 2005, Vol. 82, No. 2. |
| 82. Barriers to Naloxone Access "A more prosaic, but no less important, legal barrier to widespread naloxone access is the Food and Drug Administration’s (FDA) classification of naloxone as a prescription drug. This means that public health and harm reduction agencies cannot distribute naloxone like condoms or sterile syringes. Instead, naloxone must be prescribed by a properly licensed health care provider after an individualized evaluation of the patient. Because health care providers have to be involved, naloxone programs must deal with concerns about liability, which among doctors can be powerful even when they are not wellfounded in fact.31 The prescription status raises the cost of naloxone distribution and makes it illegal to give naloxone to lay people willing to administer the drug to others suffering an overdose." Burris, Scott; Beletsky, Leo; Castagna, Carolyn; Coyle, Casey; Crowe, Colin; and McLaughlin, Jennie Maura, "Stopping an Invisible Epidemic: Legal Issues in the Provision of Naloxone to Prevent Opioid Overdose," Drexel Law Review, Philadelphia, PA: Earle Mack School of Law, Spring 2009, Vol. 1, Number 2. |
| 83. Price of Naloxone Has Skyrocketed Since 2006 "We contribute nationally representative evidence to help answer each of these questions, including wholesale pricing data from a proprietary drug sales database spanning January 2006 to February 2017. We find that all formulations of naloxone increased in price since 2006 except for Narcan Nasal Spray. These cumulative increases totaled 2281% for the 0.4 MG single-dose products, 244% for the 2 MG single-dose products, 3797% for the 4 MG multi-dose products, and 469% for the 0.4 MG Evzio auto-injector. We believe that increased demand for naloxone from the opioid epidemic may explain the more gradual price increases for the 0.4 MG single-dose and 4 MG multi-dose products prior to 2012. On the other hand, we believe that the sudden, sustained prices increases occurring for all of the products since 2012 may be the result of a drug shortage for the 0.4 MG single-dose products and the fact that each naloxone product has historically been sold by only a single competitor." Matthew Rosenberg, Grace Chai, Shekhar Mehta, Andreas Schick, Trends and economic drivers for United States naloxone pricing, January 2006 to February 2017, Addictive Behaviors, 2018, ISSN 0306-4603, doi.org/10.1016/j.addbeh.2018.05.006. |
| 84. Naloxone Availability and Use in the US "Opioid overdose, a major source of morbidity and mortality worldwide, accounts for half of the mortality among heroin users (1) and is a leading cause of death among adults in the United States (2). Naloxone is a safe, effective, short-acting opioid antagonist for intravenous, intramuscular, subcutaneous, or intranasal administration by medical personnel and—since the late 1990s—laypersons to reverse opioid overdose. (3). Naloxone distribution is endorsed by the American Medical Association, generally integrated into preexisting services, and targeted at anyone at risk for witnessing or having an opioid overdose. Naloxone “kits” are usually wallet-sized packets containing 2 doses of naloxone and other items, including syringes, brochures, simple rescue breathing masks, and brief educational materials about overdose risks and management. As of 2010, a total of 188 U.S. programs distributing naloxone reported training 53,032 persons and recording 10,171 reversals (3)." Coffin, Phillip O., MD, and Sullivan, Sean D. PhD, "Cost-Effectiveness of Distributing Naloxone to Heroin Users for Lay Overdose Reversal," Annals of Internal Medicine 2013 Jan 1;158(1):1-9. doi: 10.7326/0003-4819-158-1-201301010-00003. |
| 85. Rapid Effect of Naloxone "Heroin is particularly toxic because of high lipid solubility, which allows it to cross the blood–brain barrier within seconds and achieve high brain levels.10 Etherington, Jeremy; Christenson, James; Innes, Grant; Grafstein, Eric; Pennington, Sarah; Spinelli, John J.; Gao, Min; Lahiffe, Brian; Wanger, Karen; Fernandes, Christopher, "Is early discharge safe after naloxone reversal of presumed opioid overdose?" Canadian Journal of Emergency Medicine, Ottawa, ON: Canadian Association of Emergency Physicians, July 2000. |
| 86. Benefits from Naloxone Distribution "Naloxone distribution to heroin users would be expected to reduce mortality and be cost-effective even under markedly conservative assumptions of use, effectiveness, and cost. Although the absence of randomized trial data on naloxone distribution and reliance on epidemiologic data increase the uncertainty of results, there are few or no scenarios in which naloxone would not be expected to increase QALYs [Quality-Adjusted Life-Years] at a cost much less than the standard threshold for cost-effective health care interventions. Ecological data, in fact, suggest that naloxone distribution may have far greater benefits than those forecast in this model: Reductions in community-level overdose mortality from 37% to 90% have been seen concordant with expanded naloxone distribution in Massachusetts (7), New York City (11), Chicago (10), San Francisco (9, 67, 68), and Scotland (69). Such a result is approached in this model only by maximizing the likelihood of naloxone use or by assuming that naloxone distribution reduces the risk for any overdose. Preliminary data showing that naloxone distribution is associated with empowerment and reduced HIV risk behaviors (70, 71) suggest that future research is needed to test these hypotheses." Coffin, Phillip O., MD, and Sullivan, Sean D. PhD, "Cost-Effectiveness of Distributing Naloxone to Heroin Users for Lay Overdose Reversal," Annals of Internal Medicine 2013 Jan 1;158(1):1-9. doi: 10.7326/0003-4819-158-1-201301010-00003. |
| 87. Cost-Effectiveness of Naloxone Distribution "Naloxone distribution was cost-effective in our base-case and all sensitivity analyses, with incremental costs per QALY [Quality-Adjusted Life-Year] gained much less than $50 000 (Table 2 and Appendix Figure 3, available at www.annals.org; see Appendix Table 3, available at www.annals.org, for detailed results of selected analyses). Cost-effectiveness was similar at starting ages of 21, 31, and 41 years; the greater QALY gains of younger persons were roughly matched by higher costs. In scenarios where naloxone administration reduced reliance on EMS, naloxone distribution was cost-saving and dominated (that is, less costly and more effective than) the no-distribution comparison. Cost-effectiveness was somewhat sensitive to the efficacy of lay-administered naloxone and the cost of naloxone but was relatively insensitive to the breadth of naloxone distribution, rates of overdose and other drug-related death, rates of abstinence and relapse, utilities, or the absolute cost of medical services. Naloxone was no longer cost-effective if the relative increase in survival was less than 0.05%, if 1 distributed kit cost more than $4480, or if average emergency care costs (as a proxy for downstream health costs) exceeded $1.1 million. A worst-case scenario, in which the likelihood of an overdose being witnessed, the effectiveness of naloxone, and the likelihood of naloxone being used were minimized and the cost of naloxone was maximized, resulted in an incremental cost of $14,000 per QALY gained. A best-case scenario, in which naloxone distribution reduced the risk for overdose, was dominant." Coffin, Phillip O., MD, and Sullivan, Sean D. PhD, "Cost-Effectiveness of Distributing Naloxone to Heroin Users for Lay Overdose Reversal," Annals of Internal Medicine 2013 Jan 1;158(1):1-9. doi: 10.7326/0003-4819-158-1-201301010-00003. |
| 88. Effectiveness of Naloxone Against Opiate Overdoses "Treatment with naloxone can reverse respiratory failure within a few minutes (Darke and Hall, 1997; Physician’s Desk Reference, 2000). Naloxone is an opiate antagonist, and is thought to displace heroin at the Mu2 receptors. Physicians and emergency personnel treat patients suspected of heroin overdose by administering an initial dose of naloxone parenterally. While 2 mg are almost always sufficient to revive a patient, additional doses can be administered if the desired improvement does not occur, and smaller doses are often used to minimize the discomfort of sudden heroin withdrawal (Physician’s Desk Reference, 2000). In adults, naloxone has a half-life of between 30 and 81 minutes (Physician’s Desk Reference, 2000). Therefore, repeated administration could be necessary to reverse the effect of particularly large or long-lasting doses of heroin. (Sporer, 1999; Physician’s Desk Reference, 2000). In practice, however, a single 2 mg does is almost always sufficient. If a patient has not taken opioids, naloxone has no pharmacological effect (Darke and Hall, 1997). "While administration of naloxone may produce acute withdrawal symptoms in patients with heroin dependence (Physician’s Desk Reference, 2000), the drug does not have long-term or life threatening adverse effects when it is administered at therapeutic doses (Strang, et al, 1996). Naloxone has been associated with complications such as seizures and arrhythmia, (Physician’s Desk Reference, 2000) but more recent research suggests that complications are exceedingly rare, that past reports of complications may have been erroneous (Goldfrank and Hoffman, 1995), or that complications occur, if at all, in patients with pre-existing heart disease (Goldfrank and Hoffman, 1995). Naloxone is not addictive, and has no psycho-pharmacological effects." Burris, Scott; Norland, Joanna; and Edlin, Brian, "Legal Aspects of Providing Naloxone to Heroin Users in the United States," International Journal of Drug Policy, 2001, Vol. 12. |
| 89. Naloxone and Overdose Prevention in the EU "In 2011, two thirds of European countries reported that ambulance personnel are trained in naloxone use; in just over half of these countries, naloxone is reported to be one of the standard medications carried in ambulances. Only Italy, Romania and the United Kingdom report the existence of community-based harm-reduction programmes that provide take-home naloxone to opioid users, their family members and carers. Legal barriers remain in place in other European countries, including Estonia, which has the highest drug-related mortality rate among adults (15–64) in the European Union. However, it was demonstrated in the United Kingdom that, with minimal training, healthcare professionals, including drug workers, can increase their knowledge, skills and confidence for managing an opioid overdose and administering naloxone (Mayet at al., 2011)." European Monitoring Centre for Drugs and Drug Addiction, "Annual report 2012: the state of the drugs problem in Europe," Luxembourg: Publications Office of the European Union, November 2012, Catalog No. TDAC12001ENC, doi:10.2810/64775. |
| 90. Marijuana and Overdose Mortality An exhaustive search of the literature finds no deaths induced by marijuana. The US Drug Abuse Warning Network (DAWN) records instances of drug mentions in medical examiners' reports, and though marijuana is mentioned, it is usually in combination with alcohol or other drugs. Marijuana alone has not been shown to cause an overdose death. Federal Drug Abuse Warning Network (DAWN); also see Janet E. Joy, Stanley J. Watson, Jr., and John A. Benson, Jr., "Marijuana and Medicine: Assessing the Science Base," Division of Neuroscience and Behavioral Research, Institute of Medicine (Washington, DC: National Academy Press, 1999); and US Department of Justice, Drug Enforcement Administration, "In the Matter of Marijuana Rescheduling Petition" (Docket #86-22), September 6, 1988, p. 57. |
| 91. Mentions of Kratom in Overdose Deaths in the US "Data on 27,338 overdose deaths that occurred during July 2016–December 2017 were entered into SUDORS, and 152 (0.56%) of these decedents tested positive for kratom on postmortem toxicology (kratom-positive). Postmortem toxicology testing protocols were not documented and varied among and within states. Kratom was determined to be a cause of death (i.e., kratom-involved) by a medical examiner or coroner for 91 (59.9%) of the 152 kratom-positive decedents, including seven for whom kratom was the only substance to test positive on postmortem toxicology, although the presence of additional substances cannot be ruled out (4). "In approximately 80% of kratom-positive and kratom-involved deaths in this analysis, the decedents had a history of substance misuse, and approximately 90% had no evidence that they were currently receiving medically supervised treatment for pain. Postmortem toxicology testing detected multiple substances for almost all decedents (Table). Fentanyl and fentanyl analogs were the most frequently identified co-occurring substances; any fentanyl was listed as a cause of death for 65.1% of kratom-positive decedents and 56.0% of kratom-involved decedents. Heroin was the second most frequent substance listed as a cause of death (32.9% of kratom-positive decedents), followed by benzodiazepines (22.4%), prescription opioids (19.7%),** and cocaine (18.4%)." Olsen EO, O’Donnell J, Mattson CL, Schier JG, Wilson N. Notes from the Field: Unintentional Drug Overdose Deaths with Kratom Detected — 27 States, July 2016–December 2017. MMWR Morb Mortal Wkly Rep 2019;68:326–327. |
| 92. Methadone-Associated Mortality "Three primary scenarios characterize current reports of methadone-associated mortality:
Center for Substance Abuse Treatment, "Methadone-Associated Mortality: Report of a National Assessment, May 8-9, 2003," CSAT Publication No. 28-03, Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, 2004. |
| 93. Medical Cannabis Laws and Opioid Overdose Mortality Rates "In an analysis of death certificate data from 1999 to 2010, we found that states with medical cannabis laws had lower mean opioid analgesic overdose mortality rates compared with states without such laws. This finding persisted when excluding intentional overdose deaths (ie, suicide), suggesting that medical cannabis laws are associated with lower opioid analgesic overdose mortality among individuals using opioid analgesics for medical indications. Similarly, the association between medical cannabis laws and lower opioid analgesic overdose mortality rates persisted when including all deaths related to heroin, even if no opioid analgesic was present, indicating that lower rates of opioid analgesic overdose mortality were not offset by higher rates of heroin overdose mortality. Although the exact mechanism is unclear, our results suggest a link between medical cannabis laws and lower opioid analgesic overdose mortality." Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical Cannabis Laws and Opioid Analgesic Overdose Mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668–1673. doi:10.1001/jamainternmed.2014.4005 |
